Aids Nursing Care Plans
Acquired immunodeficiency syndrome is a serious secondary immunodeficiency disorder caused by the retrovirus, human immunodeficiency virus . Both diseases are characterized by the progressive destruction of cell-mediated immunity with subsequent effects on humoral immunity because of the pivotal role of the CD4+helper T cells in immune reactions. Immunodeficiency makes the patient susceptible to opportunistic infections, unusual cancers, and other abnormalities.
AIDS results from the infection of HIV which has two forms: HIV-1 and HIV-2. Both forms have the same model of transmission and similar opportunistic infections associated with AIDS, but studies indicate that HIV-2 develops more slowly and presents with milder symptoms than HIV-1. Transmission occurs through contact with infected blood or body fluids and is associated with identifiable high-risk behaviors.
Persons with HIV/AIDS have been found to fall into five general categories: homosexual or bisexual men, injection drug users, recipients of infected blood or blood products, heterosexual partners of a person with HIV infection, and children born to an infected mother. The rate of infection is most rapidly increasing among minority women and is increasingly a disease of persons of color.
Can Ois Be Treated
There are many medicines to treat HIV-related OIs, including antiviral, antibiotic, and antifungal drugs. The type of medicine used depends on the OI.
Once an OI is successfully treated, a person may continue to use the same medicine or an additional medicine to prevent the OI from coming back. The Clinical Info Drug Database includes information on many of the medicines used to prevent and treat OIs.
Ocular Involvement In Hiv/aids
| add |
HIV infection can manifest in a variety of ways in and around the eyes, and these manifestations vary according to HIV disease severity, specifically, CD4+ T lymphocyte counts. In general, Kaposi sarcoma, herpes zoster ophthalmicus, candidiasis, and lymphoma are more common in earlier stages whereas tuberculosis, toxoplasmosis, and pneumocystosis occur with more impairment. Cytomegalovirus retinitis and mycobacterium-avium complex disease are usually seen in patients with profound reductions of CD4 counts. Achievement of a non-detectable HIV viral load is associated with a better prognosis.
Don’t Miss: What Type Of Infection Is Psoriasis
Avoidance Of Infectious Exposure
The following may be avoided as a preventative measure to reduce risk of infection:
- Eating undercooked meat or eggs, unpasteurized dairy products or juices.
- Potential sources of tuberculosis .
- Any oral exposure to feces.
- Contact with farm animals, especially those with diarrhea: source of Toxoplasma gondii, Cryptosporidium parvum.
- Cat feces : source of Toxoplasma gondii, Bartonella spp.
- Soil/dust in areas where there is known histoplasmosis, coccidiomycosis.
- Reptiles, chicks, and ducklings that are a common source of Salmonella.
- Unprotected sexual intercourse with individuals with known sexually transmitted infections.
Management Of Antiretroviral Therapy For Patients With Acute Opportunistic Infection

If a patient who has not been on ART develops an acute opportunistic infection, providers must decide when to initiate ART, as all patients with HIV infection should be treated expeditiously with ART. The immune augmentation that ART produces may help facilitate recovery from an acute opportunistic infection, but definitely will ultimately be beneficial in preventing HIV-related opportunistic complications and prolonging survival.71 However, complications are associated with initiation of ART, which must factor into the decision about when to initiate ART.
For ART-naïve patients, the initiation of ART may produce a clinically apparent, enhanced inflammatory response to the presenting clinical syndrome that can cause considerable morbidity.8,7274 For instance, in terms of the site of clinical disease that is being treated, initiating ART after PCP therapy is started can exacerbate pulmonary dysfunction when the enhanced immune and inflammatory responses interact with remainingPneumocystis organisms or antigen in the lung. Similarly a patient with cryptococcal or tuberculous meningitis may develop dangerously increased intracranial pressure when ART is initiated and the inflammatory response to meningeal organisms or antigen is enhanced.7278
Also Check: How To Get Ahead Of A Sinus Infection
Opportunistic Infections Free Survival Time Of Predictor Variable
The result of this study showed the OI-free survival time of patients classified as bedridden functional status was less when compared to patients classified as working active status. Additionally, adult patients with poor ART drug adherence had less OI free survival time than patients with good ART drug adherence.
|
Figure 3 KaplanMeier survival curves to compare the OIs-free survival time of PLWHIV on ART with different categories of functional status at Dessie Comprehensive Specialized Hospital from January 2015 to December 2020. |
|
Figure 4 KaplanMeier curves of OI-free survival proportion based on adherence to ART drugs at Dessie Comprehensive Specialized Hospital from January 2015 to December 2020. |
Opportunistic Infections Vs Aids
While AIDS-defining illnesses can also be classified as opportunistic infections, the opposite is not necessarily true. Opportunistic infections are those caused by otherwise common, harmless viruses, bacteria, fungi, or parasites which can cause disease when immune defenses have been compromised.
Many opportunistic infections are not life-threatening and can develop even when a persons CD4 count is high. AIDS-defining illnesses, by contrast, tend to appear during later-stage disease when the CD4 count has dropped significantly.
Some opportunistic infections, such as herpes simplex, are only considered to be AIDS-defining when they spread beyond the tissue or organ where they are typically seen.
Don’t Miss: Fungal Infection In Hiv Patient
Most Common Ois In People Living With Hiv
Since combination antiretroviral treatment for HIV became available, the number of people living with HIV who have had opportunistic infections has dropped drastically. If you start HIV treatment early and continue to take your HIV drugs as they are prescribed, you will keep your immune system strong and likely never get one of these OIs. This means you will also likely never be diagnosed with AIDS.
Some of the most common opportunistic infections in people living with HIV include:
| Opportunistic Infection |
|---|
Recommended Reading: How You Know If You Have Hiv
How Does Hiv Work
HIV is a virus that attacks CD4 cells . These white blood cells serve as helper cells for the immune system. CD4 cells send a biological SOS signal to other immune system cells to go on the offensive against infections.
When a person contracts HIV, the virus merges with their CD4 cells. The virus then hijacks and uses the CD4 cells to multiply. As a result, there are fewer CD4 cells to fight infections.
Healthcare providers use blood tests to identify how many CD4 cells are in the blood of someone who has HIV, as its one measure of the progression of HIV infection.
CDC refers to these as AIDS-defining conditions. If someone has one of these conditions, the HIV infection has advanced to stage 3 HIV , regardless of the number of CD4 cells in their blood.
Following are some of the more common opportunistic diseases. Becoming knowledgeable about these health risks is the first step in protecting against them.
Don’t Miss: Antibiotics To Treat Kidney Infection
Are Opportunistic Infections Common In People With Hiv
OIs are less common now than in the early days of HIV and AIDS when there was no treatment. Todays HIV medicines reduce the amount of HIV in a persons body and keep the immune system stronger and better able to fight off infections.
However, some people with HIV still develop OIs for reasons such as:
- they do not know they have HIV and so they are not on treatment
- they know they have HIV but are not taking ART
- they had HIV for a long time before they were diagnosed and so have a weakened immune system
- they are taking ART, but their drug combination is not working as expected and is not keeping their HIV levels low enough for their immune system to fight off infections
What Can People With Hiv Do To Prevent Getting An Oi
For people with HIV, the best protection against OIs is to take HIV medicines every day.
People living with HIV can also take the following steps to reduce their risk of getting an OI.
Avoid contact with the germs that can cause OIs.
The germs that can cause OIs can spread in a variety of ways, including in body fluids or in feces. To avoid sexually transmitted diseases or infections, use condoms every time you have sex. If you inject drugs, do not share drug injection equipment. After any contact with human or animal feces, wash your hands thoroughly with warm, soapy water.
Ask your health care provider about other ways to avoid the germs that can cause OIs.
Be careful about what you eat and drink.
Food and water can be contaminated with OI-causing germs. To be safe, do not eat certain foods, including undercooked eggs, unpasteurized dairy products or fruit juices, or raw seed sprouts.
In addition, do not drink water directly from a lake or river. For more information, read the HIV and Nutrition and Food Safety fact sheet from HIVinfo.
Travel safely.
If you are visiting a country outside the United States, avoid eating food and drinking water that could make you sick. Before you travel, read the Centers for Disease Control and Prevention fact sheet on Traveling with HIV.
Get vaccinated.
Talk to your health care provider about which vaccines you need. To learn more, read the HIVinfo fact sheet on HIV and Immunizations.
You May Like: Most Common Antibiotic For Urinary Tract Infection
How Can Opportunistic Infections Be Prevented
As these infections only occur in people with a weakened immune system, the most important way to prevent them would be to treat the underlying HIV infection. Highly Active Antiretroviral Treatment is very effective at treating HIV and ensuring the virus is adequately suppressed. With a low or undetectable viral load, the bodys immune system has time to recover and when the CD4 cells have returned to sufficient numbers, the risk of Opportunistic Infections is lowered drastically. The earlier an HIV infection is diagnosed, the earlier treatment can be started and the better the chances of avoiding Opportunistic Infections.For patients who are diagnosed with HIV later and have low CD4 counts at diagnosis , it is important to consider Opportunistic Infections prophylaxis while we are waiting for HAART to work. This means starting patients on certain medications to prevent some of these specific infections. It may take 6-12 months for the CD4 counts to recover once HAART has been initiated once the CD4 counts are improved, these prophylactic medications may be stopped.Other general advice for people living with HIV would include:
- Reducing or preventing exposure to other sexually transmitted infections
- Getting vaccinated
- Avoiding undercooked or raw foods
- Avoid drinking untreated water
- Speak to your doctor about any other changes that may need to be made at home, work, or when on vacation to reduce exposure to OIs
Take Care!
Phases Of Hiv Infection
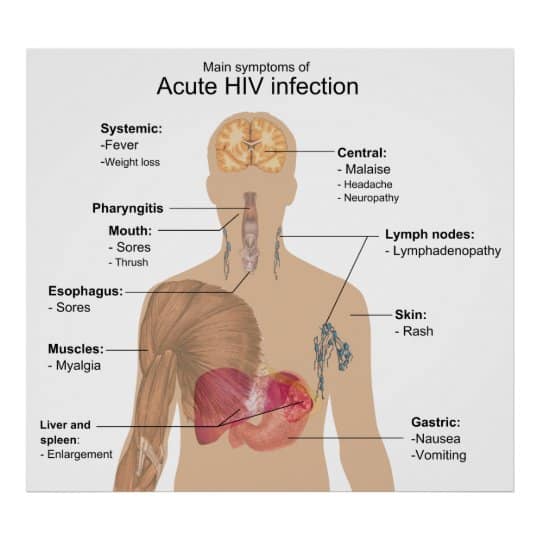
Clinical HIV infection undergoes 3 distinct phases: acute seroconversion, asymptomatic infection, and AIDS. Each is discussed below.
Acute seroconversion
Animal models show that Langerhans cells are the first cellular targets of HIV, which fuse with CD4+ lymphocytes and spread into deeper tissues. In humans, rapid occurrence of plasma viremia with widespread dissemination of the virus is observed 4 days to 11 days after mucosal entrance of the virus.
There is no fixed site of integration, but the virus tends to integrate in areas of active transcription, probably because these areas have more open chromatin and more easily accessible DNA. This greatly complicates eradication of the virus by the host, as latent proviral genomes can persist without being detected by the immune system and cannot be targeted by antivirals.
During this phase, the infection is established and a proviral reservoir is created. This reservoir consists of persistently infected cells, typically macrophages, and appears to steadily release virus. Some of the viral release replenishes the reservoir, and some goes on to produce more active infection.
The proviral reservoir, as measured by DNA polymerase chain reaction , seems to be incredibly stable. Although it does decline with aggressive antiviral therapy, the half-life is such that eradication is not a viable expectation.
Asymptomatic HIV infection
Read Also: How Long Does Hiv Fever Last
Don’t Miss: Can Pregnancy Cause Yeast Infection
Spectrum Of Hiv Disease
Acute infection with HIV causes nonspecific symptoms of viral infection and lymphadenopathy, followed by a minimally symptomatic phase during which CD4+ T lymphocyte counts decline from the normal values of 600 to 1500 cells/mm3. Below 200 cells/mm3, symptoms occur frequently from opportunistic infections, malignancies, and generalized malaise. Ocular manifestations attributable to HIV infection vary according to CD4+ T lymphocyte counts. In general, Kaposi sarcoma, herpes zoster ophthalmicus, candidiasis, and lymphoma are more common in earlier stages whereas tuberculosis, toxoplasmosis, and pneumocystosis occur with more impairment. Cytomegalovirus retinitis and mycobacterium-avium complex disease are usually seen in patients with profound reductions of CD4 counts. Achievement of a non-detectable HIV viral load is associated with a better prognosis.
Tb And Other Mycobacteriosis
The coincidence of TB and HIV epidemics has created a devastating international public health crisis. At least one-third of HIV-infected persons worldwide are infected with Mycobacterium tuberculosis, and HIV infection is, in global terms, the largest risk factor for developing TB disease . Additionally, TB is a leading cause of death for people living with HIV in low- and middle-income countries . HIV-infected persons have a substantially greater risk of progressing from latent TB infection to active TB compared with persons without HIV infection . The use of HAART has been found to be associated with a notable reduction in the risk of TB, but incidence rates remain higher than in the general population . In a study of patients initiating HAART over a follow-up period of 4.5 yrs, the risk of TB only decreased when the CD4 threshold was > 500 cells per mm3 .
Africa is experiencing the worst TB epidemic since the advent of antibiotics, with rates increasing sharply in the past two decades . Conversely, in the USA and Western Europe, a decline in the incidence of TB in HIV-infected patients has been observed in the last decades however, remarkable regional differences have been found in Europe, with rates four to seven times higher in southwest Europe than in other European regions .
Read Also: How Long Urinary Tract Infection Last
Fungal Infections Other Than Pcp
Some studies suggest a decline in the incidence of endemic fungal infections since the introduction of HAART. This is difficult to demonstrate, as the incidence of these infections has not been fully determined . The three major endemic fungi are Histoplasma capsulatum, Coccidiodes inmitis and Blastomyces dermatitidis. They are acquired by inhalation. These diseases can represent primary infection caused by exogenous exposure or reactivation of a latent focus. Infections in patients who reside outside endemic regions generally represent reactivation of latent foci of infection from previous residence in these areas . Reactivation may occur even years after moving to other geographic areas. Endemic areas include the southwest USA, northern Mexico and parts of Central and South America.
Histoplasmosis is the most common endemic mycosis in HIV patients. Most cases of disseminated histoplasmosis and coccidioidomycosis occur with CD4 lymphocyte counts â¤100 cells per mm3, but focal pneumonia is the most common in those with a CD4 cell count > 250 cells per mm3. Blastomycosis is an uncommon, but serious complication in HIV-infected persons. All of these endemic fungal infections have a wide spectrum of manifestations in HIV-infected patients with frequent lung involvement. Treatment is based on amphotericin B and triazoles .
Predictors Of Oi Among Patients Living With Hiv On Art
Residency, functional status, disclosure status, WHO clinical stage, drug adherence, taking CPT, BMI, hemoglobin level, and CD4 count were variables for multivariable analysis. Of these: functional status, WHO clinical staging, CD4 counts, and ART drug adherence were found to be significant predictors of OI. In this study, the hazard of developing OI among PLWHIV classified as bedridden at baseline was 1.6 times higher than those classified as working functional status. Similarly, the hazard of developing OI among PLWHIV classified as WHO clinical stage IV at baseline was 2.1 times higher than those classified as WHO Stages I.
On top of that, the hazard of developing OI among PLWHIV who had poor adherence was 1.7 times higher than those classified as having good adherence. KaplanMeier analysis for specific OI in different categories of adherence level showed no crossing of lines between the poor and good adherence level.
Moreover, the hazard of developing OI among HIV- positive patients who had low CD4 count at baseline was 1.92 times times higher than those categorized as CD4 count of 351 cells. The goodness of fit for the model is illustrated using a Cox-Snell residual test.
|
Figure 5 The goodness of fit test for the Cox-proportional hazard regression model. |
Don’t Miss: Can Metronidazole Treat Sinus Infection
Retinitis Infectious Necrotizing Herpetic Retinitis
Progressive outer retinal necrosis is the usual term used to describe necrotizing herpetic retinitis due to varicella zoster. It is characterized by rapid progression and minimal anterior or vitreous inflammation. There is a high frequency of no light perception in patients treated with intravenous acyclovir by one month. It often occurs in the setting of cutaneous zoster infection. There is a high incidence of retinal detachment and bilateral involvement. Intravitreal antiviral treatment or combined intravenous ganciclovir and foscarnet seem to control the infection better than intravenous acyclovir. Because of the rapidity of progression, very aggressive initial therapy is usually selected.
Do People Infected With Human Immunodeficiency Virus Have An Increased Risk Of Cancer
Yes. People infected with HIV have a substantially higher risk of some types of cancer compared with uninfected people of the same age . The general term for these cancers is “HIV-associated cancers.” Three of these cancers are known as “acquired immunodeficiency syndrome -defining cancers” or “AIDS-defining malignancies”: Kaposi sarcoma, aggressive B-cell non-Hodgkin lymphoma, and cervical cancer. A diagnosis of any of these cancers in someone infected with HIV confirms a diagnosis of AIDS.
Compared with the general population, people infected with HIV are currently about 500 times more likely to be diagnosed with Kaposi sarcoma, 12 times more likely to be diagnosed with non-Hodgkin lymphoma, and, among women, 3 times more likely to be diagnosed with cervical cancer .
In addition, people infected with HIV are at higher risk of several other types of cancer . These other malignancies include cancers of the , liver, oral cavity/pharynx, and lung, and Hodgkin lymphoma .
In addition to being linked to an increased risk of cancer, HIV infection is associated with an increased risk of dying from cancer. HIV-infected people with a range of cancer types are more likely to die of their cancer than HIV-uninfected people with these cancers .
Don’t Miss: Does Zpack Help With Sinus Infection