Baseline Characteristics Of Heart Transplantation
The baseline characteristics of patients are listed in Table . There were 29 patients with post-transplant lymphopenia on POD #7, and 29 patients without post-transplant lymphopenia on POD #7. There were no significant differences in terms of the various parameters of donors. The recipient age of the post-transplant lymphopenia group was significantly greater than that of the non-lymphopenia group . There was no significant difference between the groups in other baseline co-morbidities of recipients. Pre-transplant ALC and ALC on POD #7 were significantly lower in the post-transplant lymphopenia group than in the non-lymphopenia group . There was no significant difference in the underlying heart diseases of recipients between the groups.
Table 1 Baseline characteristics of the study population stratified by the ALC on POD #7.
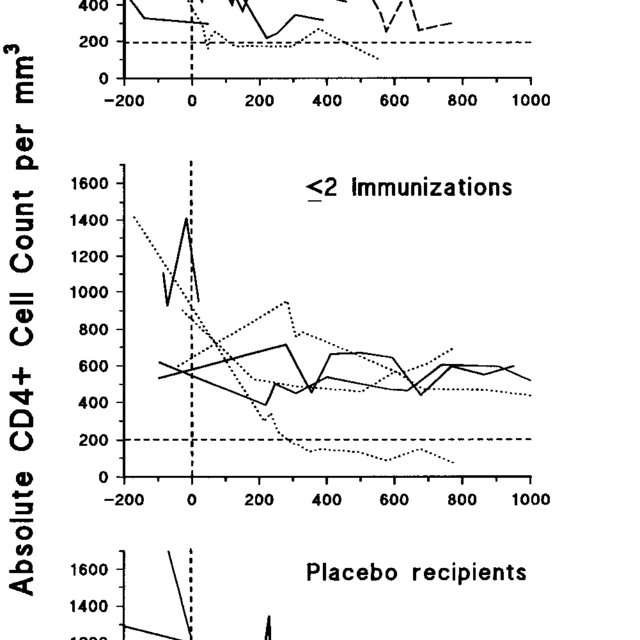
Cd4+ Trends In Hiv/hcv Co
The mean CD4+ count for the HIV/HCV participants as per the time of diagnosis of their status was 306 cells/µl while the HIV-2 /HCV participant had a mean count of 365 cells/µl. The first round of the follow-up had only 6 participants. This comprised of 4 HIV-1/HCV and two HIV-2/HCV participants with a mean count of 320 cells/µl and 297 cells/µl respectively. The second and final follow-up tests had only two male participants who were HIV-1/HCV infected their mean CD4+ count was 272 cells/µl and 171 cells/µl respectively sharing a decline of 37.1%. No HCV seroconversion was recorded among the participants throughout the follow-up period.
What Does Hiv Do To Cd4 Cells
HIV damages your immune system because it targets CD4 cells. The virus grabs on to the surface of a cell, gets inside, and becomes a part of it. When the infected CD4 cell dies, it releases more copies of HIV into the bloomstream.
Those new bits of virus find and take over more CD4 cells, and the cycle continues. This leads to fewer and fewer HIV-free, working CD4 cells.
HIV can destroy entire “families” of CD4 cells, and then the germs these cells fight have easy access to your body. The resulting illnesses are called opportunistic infections because they take advantage of your body’s lack of defense.
Recommended Reading: Sinus Infection Watery Eyes Treatment
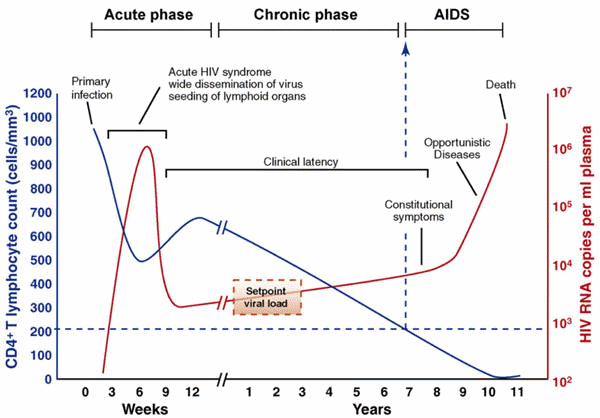
What Are The Different Stages Of An Hiv Infection
Untreated infection with HIV progresses over time and gradually impairs specific parts of the immune system, especially by destroying the white blood cells known as CD4 lymphocyte cells. This progression is described as occurring in stages. All stages require laboratory confirmation of HIV infection.
There are multiple different staging systems. For example, the Centers for Disease Control and Prevention case definition uses a staging system based on how much damage has been done to the immune system:
- Stage 1 disease is the earliest phase. Stage 1 has no unusual infections or cancers or other conditions that would be associated with AIDS. In other words, stage 1 disease has no “AIDS-defining conditions” . Although blood tests are positive for HIV, the CD4 cell count is at least 500 cells per microliter of blood .
- Stage 2 disease occurs when the CD4 count is between 200-499 cells per microliter , but again there are no AIDS-defining conditions present.
- Stage 3 disease is synonymous with AIDS and is the most severe stage. There are two ways of diagnosing stage 3 disease: either by CD4 counts below 200 cells per microliter or through documentation of an AIDS-defining condition.
Another way to conceptualize HIV is according to the characteristics or clinical manifestations: acute infection, clinical latency, or AIDS.
Cellular Dynamics Of Hiv/siv Infection
The importance of this selective targeting in AIDS pathogenesis was first demonstrated in the SIV model of pathogenesis in rhesus macaques , where it was shown that highly pathogenic, CCR5-tropic SIV infection was associated with widespread infection and massive destruction of CD4+ T cells in intestinal lamina propria and other extra-lymphoid effector sites during the first 23 weeks of infection . The wholesale destruction of CD4+ T cells in these sites has been attributed to both direct infection and Fas/Fas ligand-mediated apoptosis . Studies in HIV-infected patients have since shown a similar pattern of preferential and profound depletion of CD4+ T cells within the gastrointestinal tract during acute infection . These findings demonstrated that depletion of HIV/SIV viral targets is not slow, as originally hypothesized, but rather early and profound.
CCR5+CD4+ memory T cells are primary targets for HIV/SIV
You May Like: Mac Os Is Infected With Spyware
Absolute Lymphocyte Count Is Not A Suitable Alternative To Cd4 Count For Determining Initiation Of Antiretroviral Therapy In Fiji
Dashika A. Balak
1Reproductive Health Clinic, Ministry of Health, P.O. Box 30, Suva, Fiji
2International Union Against Tuberculosis and Lung Disease, 75017 Paris, France
3The University of Auckland, Auckland 1020, New Zealand
4Regional Public Health Service, Hutt Valley 5010, New Zealand
5Department of Health Science, College of Medicine, Nursing and Health Sciences, Fiji National University, Suva, Fiji
6Centre for International Child Health, Royal Childrens Hospital, University of Melbourne and Murdoch Childrens Research Institute, Melbourne, VIC 3052, Australia
Abstract
1. Introduction
The CD4 count is a measure of immune status in HIV-infected individuals which measures the severity of immunosuppression more accurately than clinical staging of disease. It is therefore included in international and National AIDS Programme guidelines as a threshold marker to indicate the initiation of antiretroviral therapy . However, an accurate determination of CD4 cell count requires flow cytometry which is often unavailable in resource-limited settings for a variety of reasons . If CD4 testing is not available, WHO guidelines have previously recommended using clinical staging either alone or in combination with an absolute lymphocyte count for determining ART eligibility .
2. Methods
2.1. Study Population and Setting
2.2. Data Collection and Analysis
2.3. Ethics
3. Results
| CD4 cut-off values | Number |
The Human Immune System
The immune system plays an important role to protect the host from infectious agents such as bacteria, viruses, fungi and parasites. In addition, it is also important in the identification and elimination of tumor cells as well as in response to injury and trauma. Thus, an effective and efficient immune system is essential as a host defense mechanism against infectious diseases and cancer. The immune system can be further subdivided into innate and acquired or adaptive immunity .
| Innate immunity |
| Cutaneous and mucosal immune systems |
| Mucosal membranes |
Components of the innate and acquired immune systems .
You May Like: Can You Do Root Canal On Infected Tooth
How To Recognize And Treat Acute Hiv Syndrome
BARBARA LEE PERLMUTTER, M.D., PH.D., JORDAN B. GLASER, M.D., and SAMWEL O. OYUGI, M.D., Staten Island University Hospital, Staten Island, New York
Am Fam Physician. 1999 Aug 1 60:535-542.
See related patient information handout on acute HIV syndrome, written by the authors of this article.
See related editorials on pages 407 and 411.
The diagnosis of acute human immunodeficiency virus syndrome requires a high index of suspicion and proper laboratory testing. Patients with the syndrome may have fever, fatigue, rash, pharyngitis or other symptoms. Primary HIV infection should be considered in any patient with possible HIV exposure who presents with fever of unknown cause. The diagnosis is based on a positive HIV-1 RNA level in the absence of a positive enzyme-linked immunosorbent antibody assay and confirmatory Western blot antibody test for HIV. Early diagnosis permits patient education as well as treatment that may delay disease progression. Triple-combination antiretroviral therapy should be started immediately and continued indefinitely. Compliance with medication regimens is essential to maximize benefit and discourage the development of viral resistance.
Frequency of Symptoms and Findings Associated with Acute HIV Infection
| Symptoms or findings |
|---|
HIV = human immunodeficiency virus.
Adapted with permission from Kahn JO, Walker BD. Acute human immunodeficiency virus type 1 infection. N Engl J Med 1998 339:339.
| Symptoms or findings |
|---|
Effects Of Early Initiation Of Art On B Cells
Few comprehensive studies have looked at B-cell numbers and function in HIV-infected individuals who initiate ART during the acute phase of infection. There are indications that B-cell functions, including memory B-cell responses, are impaired early after HIV infection,,. Suggestions that the early initiation of ART might reverse immune defects remain anecdotal, although early initiation of ART does seem to reverse one defect of chronic HIV infection, the low frequency of IgM+ memory B cells. Whether the restoration of normal numbers of IgM+ memory B cells translates into an improved responsiveness to T-cell-independent immunogens remains to be determined, as does the broader issue regarding the impact of early initiation of ART on the preservation of the immune system.
Read Also: What To Put On Infected Tooth
What Is It Used For
A CD4 count may be used to:
- See how HIV is affecting your immune system. This can help your health care provider find out if you are at higher risk for complications from the disease.
- Diagnose AIDS
- The names HIV and AIDS are both used to describe the same disease. But most people with HIV don’t have AIDS. AIDS is diagnosed when your CD4 count is extremely low.
- AIDS is the most severe form of HIV infection. It badly damages the immune system and can lead to opportunistic infections. These are serious, often life-threatening, conditions that take advantage of very weak immune systems.
You may also need a CD4 count if you’ve had an organ transplant. Organ transplant patients take special medicines to make sure the immune system won’t attack the new organ. For these patients, a low CD4 count is good, and means the medicine is working.
Initial History And Physical Examination
The goal of the initial history and physical examination is to assess for clinical manifestations of HIV infection and related conditions. The initial history should elicit details about sexually transmitted infections, hepatitis, substance use, and sexual practices. It should include any history of previous HIV treatment and information about the patient’s family and social networks. Except in cases of acute or advanced HIV infection, the initial physical examination generally shows no HIV-related manifestations. The presence of thrush, oral or anogenital ulcers or warts, lymphadenopathy, rashes, or skin lesions should prompt further evaluation,11 especially when persistent or substantial immunosuppression is present .
Don’t Miss: Can A Urinary Tract Infection Heal On Its Own
Immunologic Changes In Hiv Infection
3.3.1. Depletion of CD4+T cells causes immunodeficiency
Untreated HIV-1 infection is associated with a gradual loss of peripheral CD4+ T cells. Loss of CD4+ T cells and systemic immune activation are the major hallmarks of HIV infection . There are two major phases of HIV disease, acute and chronic infection. Acute infection is associated with gradual loss of CD4+ T cells in the mucosal tissue while chronic infection is characterized by immune activation which is associated with massive production of proinflammatory cytokines . This subsequently leads to decrease in peripheral CD4+ T cells and profound immunodeficiency.
The major mechanism of CD4+ T cell depletion in HIV patients is due to apoptosis, in which the number of apoptotic cells exceed the number of HIV-infected cells . Other causes of CD4+ T cell depletion include impairment of de novo production of T lymphocytes by the thymus , induction of syncytium formation, alteration of membrane permeability, mitochondrial dysfunction as well as killing by HIV-specific CD8+ T cells due to immune activation .
3.3.2. Loss of function of CD4+ T cells
Binding of gp120 to newly synthesized intracellular CD4+ T cells that result in the interference of normal protein processing in the endoplasmic reticulum as well as block the surface expression of CD4+ T cells.This makes the cell incapable of responding to antigenic stimulation and,
3.3.3. Cytokine dysregulation and coagulopathy in HIV infection
3.3.3.1. Cytokine dysregulation
Immunological And Haematological Changes In Hiv Infection
Submitted: July 1st, 2014Reviewed: July 24th, 2015Published: September 2nd, 2015
DOI: 10.5772/61259
There are two ways to cite this chapter:
There are two ways to cite this chapter:
Total Chapter Downloads on intechopen.com
Overall attention for this chapters
- School of Dental Sciences, USM Health Campus, Kubang Kerian, Kelantan, Malaysia
Wan Suriana Wan Ab Rahman
Suhair Abbas Ahmed Al-Salih
Che Maraina Che Hussin
You May Like: Can You Fight Infection Without Antibiotics
How Are T Cells Linked To Hiv And Aids
HIV enters its genetic information into helper T cells to make copies of itself. When this happens, the helper T cells die. This severely disrupts the immune response. Low levels of helper T cells mean killer T cells and other white blood cells do not receive as much information about pathogens in the body. As a result, disease-causing bacteria and viruses multiply with minimal detection.
When the amount of helper T cells falls below 200 cells/mm3 , a person may receive an AIDS diagnosis. But healthcare professionals will also take into account other variables such as overall white blood cell count and the percentage of lymphocytes.
AIDS is the most severe stage of HIV. When a person receives an AIDS diagnosis, their immune system is severely compromised, and they are at risk for opportunistic illnesses. The survival rate without treatment at this stage is typically
200 cells/mm3 , they will likely receive an AIDS diagnosis.
When a person has HIV, a healthcare professional will collect a blood sample and request a CD4 count. The CD4 count helps determine how many helper T cells a person has.
But when analyzing a CD4 count, healthcare professionals must take into account that:
- CD4 levels could be lower in the morning
- stress and fatigue may affect CD4 levels
- corticosteroid levels could increase or decrease CD4 levels
The CD4 count helps healthcare professionals monitor HIV progression and if the person is at risk for opportunistic illnesses.
100â150cells/mm3 after 1 year.
What Do The Results Mean
CD4 results are given as a number of cells per cubic millimeter of blood. Below is a list of typical results. Your results may vary depending on your health and even the lab used for testing. If you have questions about your results, talk to your health care provider.
- Normal: 500â1,200 cells per cubic millimeter
- Abnormal: 250â500 cells per cubic millimeter. It means you have a weakened immune system and may be infected with HIV.
- Abnormal: 200 or fewer cells per cubic millimeter. It indicates AIDS and a high risk of life-threatening opportunistic infections.
While there is no cure for HIV, there are different medicines you can take to protect your immune system and can prevent you from getting AIDS. Today, people with HIV are living longer, with a better quality of life than ever before. If you are living with HIV, it’s important to see your health care provider regularly.
Don’t Miss: B12 Shots For Sinus Infection
Cd4+ Lymphocyte Count Trends In Hiv
The mean CD4+ lymphocyte count of males and females as per the diagnoses of their HIV status was 375 cells/µl and 291 cells/µl respectively.
Only 4 out of the 7 men and 25 women participated in the first round of the follow-up test six months later. The mean CD4+ lymphocyte count for the 4 male participants was 464 cells/µl and 339 cells/µl for the 25 females. During the second round of the follow-up test 12 months later only three males and 18 females participated. The mean CD4+ count of these was 328 cells/ and 303 cells/ for male and females respectively. There was a 29.3% and 10.6% decline in the mean CD4+ count of the male and female participants over the 6-month interval. Similarly, the last round of the follow-up test had only 2 male and 10 female participants and their mean CD4+ count was 316 cells/µl and 285 cells/µl for male and females respectively. The cumulative decline in CD4+ of the participants who fully completed the programme was 43.2% and 44.4% for male versus female respectively. A highly significant was found between CD4dx and the declining CD4 trends when CD4dx was regressed against, the first, second and third CD4 counts however, no such association was found between CD4 counts and age or sex due in large part to the small number of participants who completed the programme.
The Classification Of Hiv Disease
The staging and classification of HIV disease are standard tools for monitoring HIV epidemic and also serve as a guide for clinicians in managing HIV patients. It provides important information for patients and clinicians regarding the staging of HIV disease and clinical management. Currently, two major classification are used: World Health Organization Clinical Staging and Disease Classification System and the United State Centers for Disease Control and Prevention Classification System.
The WHO Clinical Staging and Disease Classification System is usually used in resource-constrained settings without access to CD4 cell count measurements or other diagnostic and laboratory methods The system classifies the HIV disease based on the clinical manifestations of patients. By contrast, the CDC classification system assesses the HIV disease severity by CD4 cell count as well as by the presence of specific HIV-related conditions . This classification system is usually beneficial in the clinical as well as epidemiologic research.
3.2.1. WHO clinical staging of HIV/AIDS and case definition
Also Check: Planned Parenthood Treat Yeast Infections
Study Population And Sample Collection
A total of 1500 people age 11 months to 76 years referred for HIV serology at the Royal Victoria Teaching Hospital, Banjul, The Gambia between the months of July and December 2002 were counseled on a one to one basis. Following informed consent, 10 ml of venous blood was drawn from each participant. Samples from pregnant women were collected during their registration visit to the antenatal clinic irrespective of their trimester of pregnancy. 2 ml of each blood sample was dispensed into an EDTA container for CD4+ count. The remaining was centrifuged and the serum separated and frozen in two aliquots. One aliquot was preserved at 20°C for short-term use and the other at 70°C. No patient was aware of his HIV status prior to the visit to the hospital. Data on patient’s demographic characteristics and behavioural factors were obtained in a one to one personal interview.