Gum Tenderness And Swelling
Here are some swelling symptoms that may point to root canal infections:
- Swelling that lasts for a long period of time
- A gum pimple-like boil situated in front of or on the root tip
- The tooth that feels a bit taller than adjacent teeth
- A recurring pimple that forms on the gums
- Pronounced swelling.
What Damages Tooth Pulp
Tooth pulp is the live tissue inside your teeth. Most of us can go for years without even thinking about tooth pulp until you experience dental discomfort or pain. Tooth pulp can become infected or inflamed when the tooth undergoes repeated dental procedures. Tooth injuries and severe tooth decay can also damage the dental pulp in your teeth.
What Happens During The Procedure
Most dentists will use anesthesia during the procedure to numb the mouth. It is often inserted into the gums via an injection. From there, a small hole is drilled into the top of the infected tooth, and the diseased pulp is cleaned out with files.
The dentist will also clear out the canals that run through the tooth to ensure all infected sections are removed. Afterward, an antibiotic may be applied before the affected area is filled and sealed.
Read Also: Antibiotics For Uti Bladder Infection
Causes Of Dental Abscess After Root Canal
Basically, tooth abscess is pus formation, which can be attributed to bacterial infection that has accumulated in the soft pulp of the tooth. In the case of a root canal, it can occur when the procedure is not carried out properly, or when a faulty crown is used. Discussed below are the most prominent causes of tooth abscess after the root canal procedure that you need to be aware of.
Why Get A Root Canal
Your dentist will recommend a root canal once the decay on a tooth reaches the pulp. Made up of blood vessels and nerves, the pulp is the trigger for the pain. Sometimes, trauma can happen to the tooth that leads to discoloration or abscess. In these cases, even without a considerable amount of day, you might still need to get a root canal.
Read Also: Medication For Middle Ear Infection
Can A Tooth With A Root Canal Get Infected
Many people fear the day that they will be told that they need a root canal, having had a reputation as a painful procedure. But with the latest techniques, root canals do not have to be this way. Although it usually has favorable results, there are times when infections develop. Why does this happen? Read on as we take a closer look at this common dental procedure.
Perform The Root Canal
Doing the root canal can help in draining the abscess and be the determining factor of saving the tooth. A dentist completes this by drilling into the tooth and removing the bacteria-filled area. After ensuring that the abscess is drained and clear, the dentist will perform the seal. The seal of a root canal will ensure that no bacteria or other debris gets in the chamber of the tooth which could be painful and cause other issues to arise.
Don’t Miss: How To Reduce Swelling From Yeast Infection
What Are The Alternatives To Root Canal Treatment
The only alternative to root canal therapy is tooth removal. Even though its best to save natural teeth whenever possible, extraction may be necessary to preserve your oral health.
If youre not a good candidate for root canal treatment, the tooth can be extracted and replaced with a dental implant, dental bridge or partial. To learn more about root canal vs extraction, call your healthcare provider.
Why You May Need Retreatment After A Root Canal
Even when every step of the procedure goes smoothly, a tooth that is treated with a root canal may experience prolonged sensitivity or reinfection. According to the American Association of Endodontists , certain circumstances may prevent a tooth treated with a root canal from healing properly:
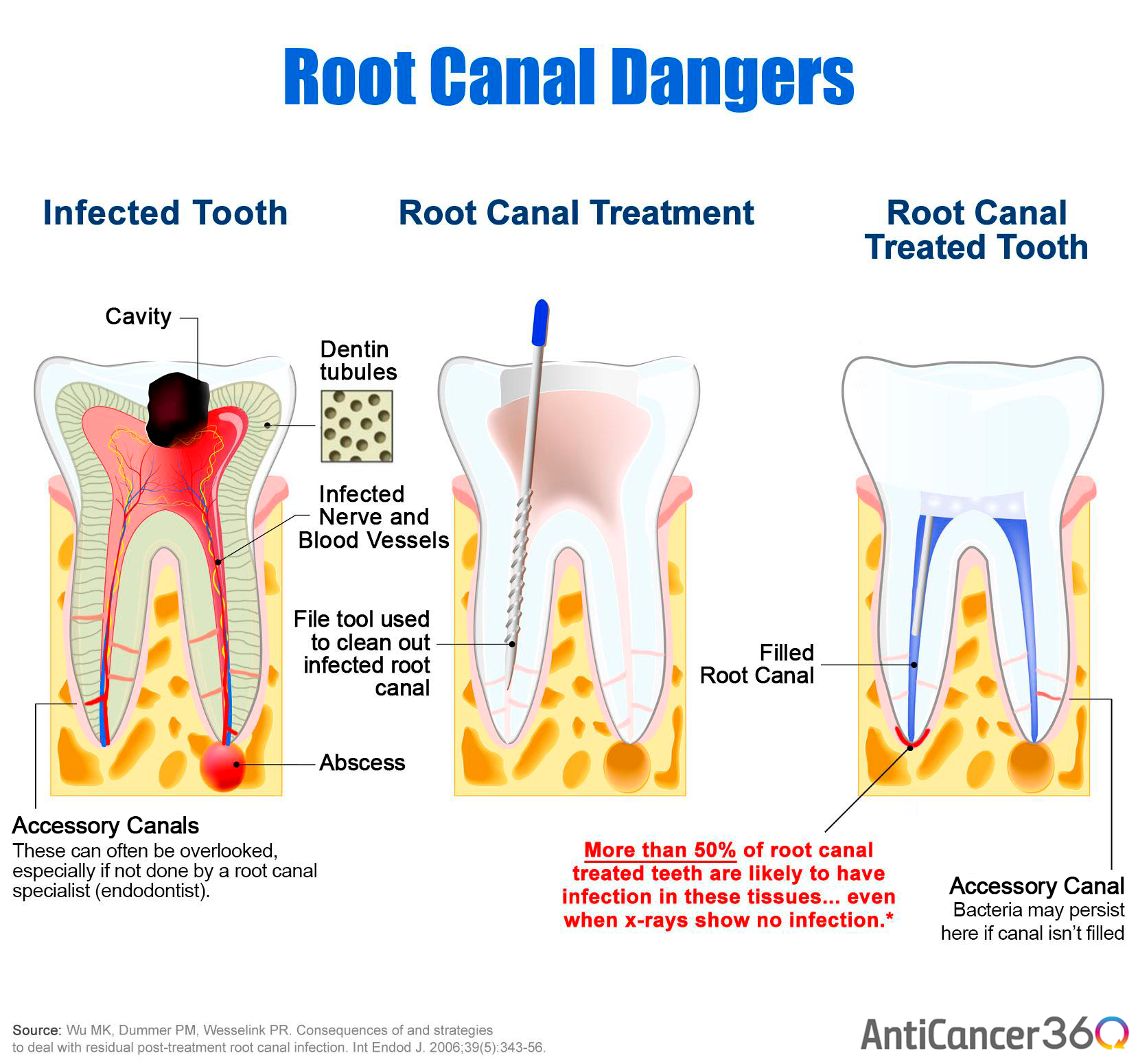
- If the dental professional misses tiny, hidden canals or curved canals during the first treatment, the bacteria inside them may not be entirely removed and can cause infection.
- Immediately after the root canal, the dental professional often places a temporary filling to provide a short-term seal for the root canal before placing the permanent restoration . If there is a delay in placing the permanent restoration, there is a greater chance that the root canal can get reinfected.
- If bacteria in the saliva get under the filling material before the filling is placed, the canal can become reinfected.
- If the patient doesn’t maintain proper oral hygiene, new cavities can form on the same tooth that already received a root canal.
- A filling or crown placed on the tooth that received the root canal can crack, loosen or break, allowing a new infection to start.
Recommended Reading: Types Of Antibiotics For Bladder Infection
What If I Have An Infection Before The Root Canal
If you are experiencing an infection before your root canal procedure is performed, you may have an antibiotic prescribed to you in order to treat the infection. If you have an active infection during root canal therapy, there is a chance the infection can block the anesthetic from working and numbing the area. It is important to talk with your dentist about your symptoms, and follow their recommendations for treating the infection first, then the full tooth.
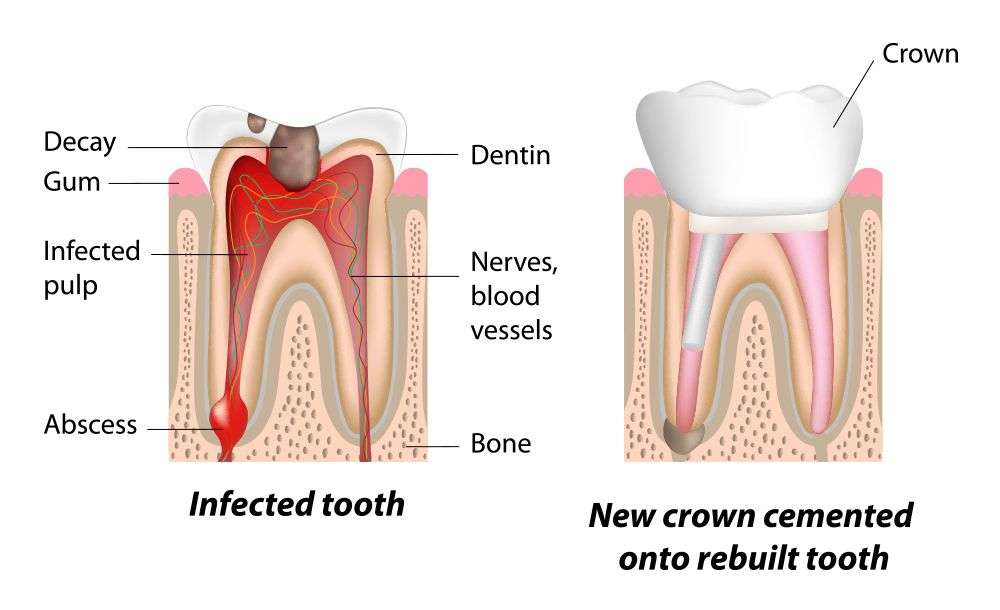
What Happens During A Root Canal
For the first step of this procedure, Dr. Dyras numbs the area around your tooth, removes any decayed tooth material, and creates a channel to access the root’s interior. Dr. Dyras will then remove the infected nerve tissue from the root, and flush and clean the area.
Next, the root is filled with a special sealing material, and a supporting post or posts are placed inside the tooth. The tooth interior is then built up with composite, which is bonded and hardened using a special curing light.
With the tooth built up and cured, Dr. Dyras will finish preparing the tooth for the crown. An impression is taken of the prepared tooth and sent to a dental laboratory. A temporary crown is put in place while the final version is being crafted.
At a subsequent appointment, Dr. Dyras will remove the temporary crown and replace it with the final restoration. Once completed, your tooth is now restored to optimal shape and function.
Read Also: Infected Gum Around One Tooth
What Should One Expect After Root Canal Therapy
Root canal therapy should relieve the pain you feel. Until your root canal procedure is completely finished — that is, the permanent filling is in place and a crown, if needed, is in place — it’s wise to minimize chewing on the tooth under repair. This step will help avoid recontaminating the toothâs interior and also may prevent a fragile tooth from breaking before the tooth can be fully restored.
For the first few days following the completion of treatment, the tooth may feel sensitive due to natural tissue inflammation, especially if there was pain or infection before the procedure. This sensitivity or discomfort usually can be controlled with over-the-counter pain medications such as ibuprofen or naproxen . Most patients can return to their normal activities the next day.
As far as oral health care is concerned, brush and floss as you regularly would, and see your dentist at normally scheduled intervals. Because the final step of root canal therapy is application of a restoration such as a crown or a filling, it will not be obvious to onlookers that a root canal was performed.
Root canal treatment is highly successful the procedure has more than a 95% success rate. Many teeth fixed with root canal therapy can last a lifetime.
Can An Infection Spread To The Gums Or To Other Teeth
Like any other infection, a root canal infection can spread to surrounding tissue in the mouth, including other teeth, gums, and tissue in the cheeks and face.
The infection wont go away until its treated, and the longer you wait, the farther it can spread.
How far the infection spreads depends on how soon you get it treated after you start noticing symptoms. If you seek treatment hours or a couple of days after the infection starts, the spread can be minimized to the tooth itself or the surrounding teeth and tissues.
A root canal infection thats left untreated can spread far beyond the tooth. In some cases, the infection can spread to the jaw, the face, and even into the bloodstream.
Also Check: Natural Treatment For Tooth Infection
What Are Root Canal Infections
Teeth arent solid all the way through theyre made up of layers. The hard, outer surface of a tooth is called enamel. The inner layer is called dentin and is a porous, almost sponge-like tissue. At the center of each tooth is a collection of soft tissue called pulp.
The pulp contains the nerves and blood vessels that allow the tooth to grow. Its full of cells called odontoblasts that keep the tooth healthy.
A root canal removes the pulp of a tooth thats been infected or damaged by tooth decay or other injuries. Root canals can save teeth and are considered very safe.
Root canal infections arent common, but theres a small chance of a tooth becoming infected even after a root canal is performed.
Overview Of A Root Canal
To fully understand the purpose of a root canal treatment, it helps to get a good grasp of the tooths anatomy. The first layer of the tooth, known as the enamel, encases another layer called the dentin, which contains soft tissues called the pulp. The tooth pulp comprises the nerves, blood vessels and connective tissues, and plays an important role during the eruption in developing the surrounding hard layers of the tooth.
The tooth pulp runs from the tooth crown to the tip of the root. It is important while the tooth is still growing. However, after the tooth fully forms, it can survive independent of the pulp.
A person will need a root canal treatment if the pulp chamber of the tooth becomes infected or inflamed. This may be due to severe tooth decay, tooth cracking and other forms of tooth damages. Without treatment, pulp infection can cause severe pain or cause a tooth abscess, which often necessitates tooth extraction.
There are visible signs that a person needs to undergo root canal surgery. The most obvious one is pain, as well as sensitivity to hot or cold items, pain when chewing or touching, discoloration, swelling and inflammation of the lymph nodes. Patients may also notice pimple-like swelling on their gums. However, these symptoms are not the same for everyone some people may show no symptoms, yet need to undergo a root canal treatment to prevent additional damage and save the tooth.
Don’t Miss: Ear Infection Hurts So Bad
What Causes Infection After A Root Canal
A tooth may become re-infected for a number of different reasons. One possibility is that the permanent crown meant to add further protection against decay may have been delayed, giving bacteria a chance to re-infect the tooth. It is also possible the original seal after filling wasnt sufficient to prevent bacterial contamination.
What Is An Abscessed Tooth
Youll know your tooth is abscessed when you feel an ache in the bone around the tooth. Other symptoms of an abscessed tooth include swelling or redness of the gums, painful gums, fever, and having a bad taste in your mouth. If you recognize these signs you need a root canal, we recommend calling your dentist to schedule an emergency appointment.
Abscessed teeth happen when your tooth has decayed enough for infection to breach the dental pulp inside your tooth. Once the tooth pulp is infected, it can create an abscess in the gums around the tooth. An abscess is a swollen area in your gums that contains pus.
If left untreated, an abscessed tooth can cause the tooth and jawbone to deteriorate, creating further pain and damage to your smile. The abscess can also push the tooth upwards, making it looser and more vulnerable to falling out.
Don’t Miss: Strep Throat And Ear Infection
Have More Questions About Root Canals And Infected Teeth
Have more questions about root canals and how they can help with an infected tooth? Give our office a call, and we will gladly answer any additional questions you may have. Contact us today!
Request an appointment here: or call Marion Family Dental at for an appointment in our Marion office.
Can Antibiotics Heal An Infected Root Canal
Oral health plays a vital role in overall health. Poor oral health can lead to many other physical health conditions in addition to gum or tooth problems. When you have tooth pain such as a tooth infection, antibiotics can go a long way in helping to address the infection, but unfortunately, antibiotics cannot completely heal an infected tooth.
Whats more, if youre dealing with an infected root canal, antibiotics really are not going to cut it. In these cases, youll need to have the bacteria removed, either by root canal treatment or tooth extraction, in order for it to heal. Why is that, and more importantly, what can be done to take care of the infection once and for all?
You May Like: Can You Treat A Kidney Infection At Home
Treatment Of Root Canal Re
Your dentist will investigate more to confirm the source of the pain. An X-ray will be the most useful tool here. It can be a small X-ray film placed in the mouth or a big X-ray machine to see more detail in a 3-dimensional view.
Besides, the dentist will likely find out the reason for the re-infection after the root canal. The reasons can be grouped into three categories:
What Happens If You Need A Root Canal But Dont Get One

Root canals are a huge help to teeth that are infected, injured, or damaged. Not getting a root canal can expose the tooth to increasing infectious bacteria and further damage due to weakness at the core of the tooth.
Dont opt for a tooth extraction as an alternative to root canals, even if you hope itll be less painful.
Root canals have become less painful in recent years due to advances in anesthesia and pain medication. Pulling out teeth unnecessarily can damage the structures of your mouth and jaw.
Also Check: Can Sinus Infection Make Your Head Feel Weird
Why Does The Pulp Need To Be Removed
When pulp is damaged, it breaks down, and bacteria begin to multiply within the pulp chamber. The bacteria and other dying pulp remnants can cause an infection or abscessed tooth. An abscess is a pus-filled pocket that forms at the end of a toothâs root. In addition to an abscess, an infection in the root canal of a tooth can cause:
One Size Does Not Fit All
After reading the above, Im sure you can see that with root canals, one approach does not fit every situation or patient. its impossible to generalize about whats best for each individual. Every situation is different, including patients overall oral health, wants, needs, history, symptoms and the condition of the tooth itself. Many alternative doctors in the holistic and integrative health field believe that every root canal should be extracted no matter what. This, in my experience, is not accurate or realistic, as it takes a very complex issue like health and generalizes one approach for every patient and situation. Conversely, most dentists and root canal specialists recommend that the tooth try to be saved at all costs. This is also not practical or realistic in some cases, as the tooth is clearly not a good prospect for additional treatment.
Also Check: Cure Yeast Infection Without Medication
Resolving Pain With Root Canals
The dental issues that cause the need for root canals often make patients uncomfortable. At the bare minimum, patients will experience an excruciating toothache. These toothaches may be spontaneous, occurring even when the patient is not using the tooth. Eventually, this may evolve into a severe headache. Many patients often do not make the connection between the toothache and the headache.
A tooth that is still alive will also be sensitive to heat and cold, even after the patient has removed the stimulus. The tooth may be particularly susceptible to heat sensitivity. Patients with teeth that are already dead and have become abscessed will cause pain when the patient chews or otherwise puts pressure on the tooth. Any abscesses may produce swelling or bleeding, even to the point of requiring emergency care.
How A Root Canal Can Save The Tooth
During the procedure, the dentist will remove the infected or inflamed pulp material and clean the pulp chamber and root canal properly. After disinfecting the area, the dentist will fill the gap with a filling material called gutta-percha. Afterward, the next step is to cover the affected tooth with a crown to strengthen and protect it from damages.
The tooth will look and feel natural and will continue to function fully for many years to come. Without the recommended root canal treatment, there is a risk that the infection will spread further and may lead to swelling and jawbone infection, which can be detrimental to overall wellbeing. At that point, there will be no other alternative than to remove the tooth.
Read Also: Will Bladder Infection Go Away On Its Own