Hiv In The United States
About 1.2 million people in the United States have HIV. In 2018, nearly 38,000 people received an HIV diagnosis in the United States and dependent areas. Though the number of new HIV diagnoses has declined over the last few years, the number of people who have HIV has been increasing because people with HIV are now living longer.
In 2018, 81% of new diagnoses in the United States and dependent areas were among adult and adolescent men and 19% were among adult and adolescent women. Most new HIV diagnoses among women were from heterosexual contact , and another 15% were from injection drug use. By age, 21% of new HIV diagnoses in 2018 were among young people aged 13 to 24, 36% were among people aged 25 to 34, 19% were among people aged 35 to 44, 14% were among people aged 45 to 54, and 10% were among people aged 55 and older.
When you live in a community where many people have HIV infection, the chances of having sex with someone who has HIV are higher. This interactive atlas allows you to see the rates of HIV infection in different US communities. Within any community, the prevalence of HIV can vary among different populations.
Overall, data show
Rationale For Treatment Of Acute Hiv Infection
The potential benefits of initiating antiretroviral therapy for patients with acute and recent HIV infection include accelerated resolution of symptomatic acute retroviral syndrome, minimized immunologic damage, diminished size of the latent HIV reservoir pool, and prevention of HIV transmission to others.
Initial Inoculation Of Hiv
The immunopathogenesis of acute HIV infection is best understood with regard to transmission via the genital mucosa. Studies of intravaginal inoculation of simian immunodeficiency virus in rhesus monkeys helped generate a model for early events of human sexual transmission of HIV . In the proposed model, HIV first infects Langerhans cells . On the surface of the Langerhans cell, HIV initially binds to the CD4 molecule, followed by binding to the CCR5 cellular coreceptor the Langerhans cells express CCR5 coreceptors, but usually not CXCR4 coreceptors. Most often, the transmitted HIV is macrophage-tropic HIV , which preferentially binds to the CCR5 coreceptor.
Don’t Miss: How To Avoid A Yeast Infection While Taking Antibiotics
Testing For Recent Hiv Infection
For individuals with a positive HIV antibody test and suspected recent infection, it is important to try and determine the last negative HIV test. In this setting, a negative HIV-1/2 antigen-antibody immunoassay in the prior 6 months would support a diagnosis of recent HIV infection. From a research standpoint, the detuned HIV antibody assay could confirm recent infection, but this test is not widely available in clinical settings.
How Did The Patient Develop Acute Hiv Infection What Was The Primary Source From Which The Infection Spread
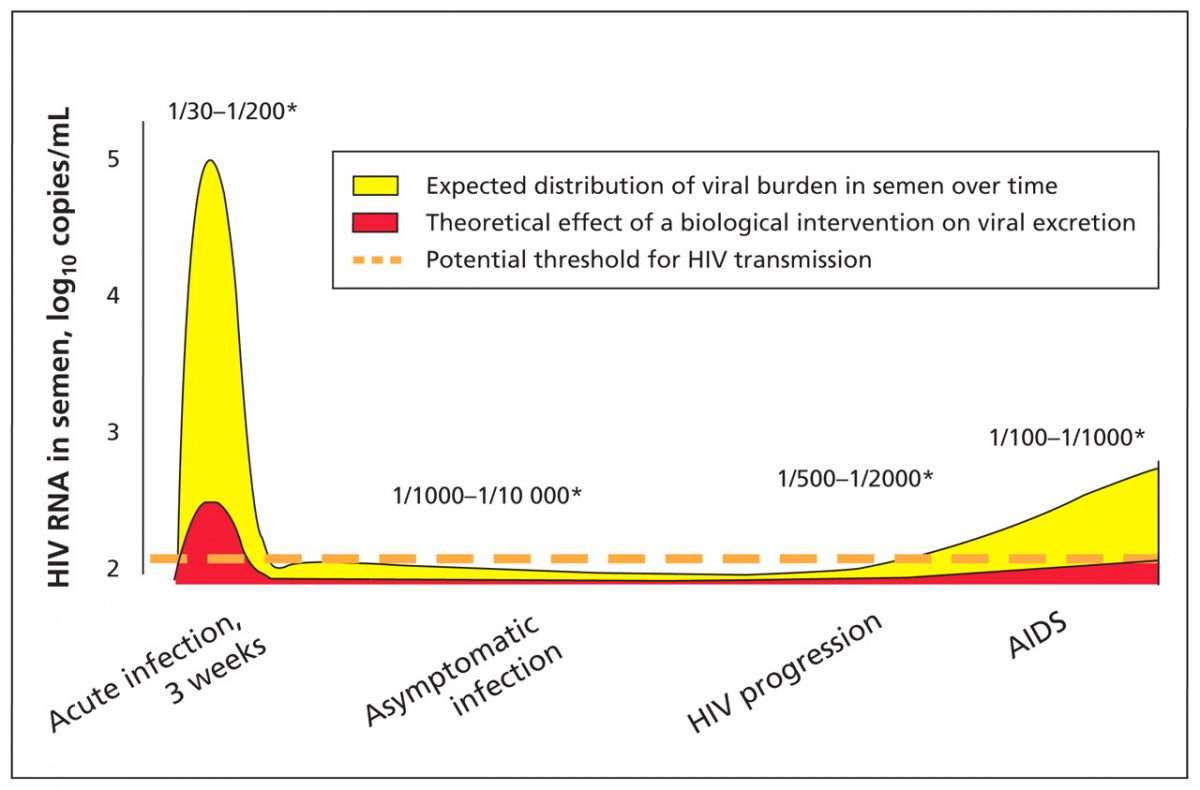
HIV is primarily transmitted by contact of bodily fluids with mucosal membranes. The likelihood of transmission is directly related to both the volume of fluids a person is exposed to and the level of virus present within the fluids. Bodily fluids that contain significant amounts of infectious HIV are blood, vaginal and seminal fluids, cerebrospinal fluid, and breast milk. The level of HIV present in other bodily fluids, such as sweat, tears, and saliva, is very low.
Sexual exposure
Transmission can occur any time vaginal or seminal fluids come in contact with mucous membranes .It is noteworthy that sexual transmission frequently occurs from those unaware of their infection status. Moreover, those with acute infection may contribute disproportionately to transmission events, since these people are engaging in high risk activity, are unaware of their infection status, and tend to have high levels of virus in blood and genital secretions.
Blood exposure
The risk of transmission in this setting is directly related to the amount of blood a person is exposed to, the amount of virus present in the blood, and in the setting of needle sticks to the level of penetration into the skin.
HIV-infected pregnant or nursing mothers
Household contacts
Recommended Reading: What Antibiotic Is Good For Ear Infection
Acute Human Immunodeficiency Virus Infection Syndrome
Medical Definition Of Acute Hiv Infection
- Medical Editor: Melissa Conrad Stöppler, MD
Reviewed on 3/29/2021
Acute HIV infection: The body’s initial reaction to infection by the HIV virus. Acute HIV infection is a flu-like syndrome that occurs immediately after a person contracts HIV . The syndrome is characterized by fever, sore throat, headache, skin rash and swollen glands .
This syndrome precedes seroconversion — the development of detectable antibodies to HIV in the blood as a result of the infection. It normally takes several weeks to several months for antibodies to the virus to develop after HIV transmission. When antibodies to HIV appear in the blood, a person will test positive in the standard ELISA test for HIV.
Don’t Miss: Natural Antibiotics For Dental Infection
Protocol For Rapid Art Initiation
|
References
Abdool Karim SS, Naidoo K, Grobler A, et al. Timing of initiation of antiretroviral drugs during tuberculosis therapy. N Engl J Med 2010 362:697-706.
Boulware DR, Meya DB, Muzoora C, et al. Timing of antiretroviral therapy after diagnosis of cryptococcal meningitis. N Engl J Med 2014 370:2487-2498.
Ford N, Migone C, Calmy A, et al. Benefits and risks of rapid initiation of antiretroviral therapy. AIDS 2018 32:17-23.
Torok ME, Yen NT, Chau TT, et al. Timing of initiation of antiretroviral therapy in human immunodeficiency virus associated tuberculous meningitis. Clin Infect Dis 2011 52:1374-1383.
WHO. Guidelines for managing advanced HIV disease and rapid initiation of antiretroviral therapy. 2017
Dhhs Guidelines For Antiretroviral Agents
Current Guidelines for the Use of Antiretroviral Agents in HIV-1Infected Adults and Adolescents, published by US Department of Health and Human Services, recommend starting antiretroviral therapy for all individuals when infection is diagnosed, regardless of stage of infection, as long as barriers to therapy do not exist. Considerations are as follows:
-
The goal of treatment should be the suppression of plasma HIV RNA to below detectable levels
-
Testing for plasma HIV RNA levels and CD4 count and toxicity monitoring should be performed
-
If therapy is initiated before drug-resistance test results are available, a ritonavir-boosted protease inhibitorbased regimen should be used, because clinically significant resistance to protease inhibitors is less common than resistance to non-nucleoside reverse transcriptase and integrase inhibitors in antiretroviral therapynaive persons who harbor drug-resistant virus.
Read Also: Best Tea For Tooth Infection
How This Guideline Was Developed
This guideline was developed by the New York State Department of Health AIDS Institute Clinical Guidelines Program, which is a collaborative effort between the NYSDOH AI Office of the Medical Director and the Johns Hopkins University School of Medicine, Division of Infectious Diseases.
Established in 1986, the goal of the Clinical Guidelines Program is to develop and disseminate evidence-based, state-of-the-art clinical practice guidelines to improve the quality of care provided to people with HIV, hepatitis C virus, or sexually transmitted infections people with substance use issues and members of the LGBTQ community. NYSDOH AI guidelines are developed by committees of clinical experts through a consensus-driven process.
Medical Care Criteria Committee for adult HIV care guidelines: The NYSDOH AI charged the MCCC with developing evidence-based recommendations for clinicians in NYS who provide care to individuals with HIV. The purpose of the Diagnosis and Management of Acute HIV Infection clinical practice guideline is to guide clinicians in NYS who provide ambulatory, inpatient, and emergency medical care for adults 18 years old who present with signs or symptoms of acute HIV infection.
Committee role: Committee members actively participate in guideline development, including evidence review, drafting of recommendations and text, manuscript review, consensus approval of all recommendations, and rating of recommendations.
MCCC Writing Group
Rationale For Rapid Art Initiation
|
References
Amanyire G, Semitala FC, Namusobya J, et al. Effects of a multicomponent intervention to streamline initiation of antiretroviral therapy in Africa: a stepped-wedge cluster-randomised trial. Lancet HIV 2016 3:e539-e548.
CDC. Understanding the HIV care continuum. 2018
CDC. Monitoring selected national HIV prevention and care objectives by using HIV surveillance dataUnited States and 6 dependent areas, 2017. 2019 Jun.
Coffey S, Bacchetti P, Sachdev D, et al. RAPID antiretroviral therapy: high virologic suppression rates with immediate antiretroviral therapy initiation in a vulnerable urban clinic population. AIDS 2019 33:825-832.
Cohen MS, Chen YQ, McCauley M, et al. Antiretroviral therapy for the prevention of HIV-1 transmission. N Engl J Med 2016 375:830-839.
Colasanti J, Sumitani J, Mehta CC, et al. Implementation of a rapid entry program decreases time to viral suppression among vulnerable persons living with HIV in the Southern United States. Open Forum Infect Dis 2018 5:ofy104.
Ford N, Migone C, Calmy A, et al. Benefits and risks of rapid initiation of antiretroviral therapy. AIDS 2018 32:17-23.
NYCDHMH. HIV surveillance annual report, 2017. 2018
Recommended Reading: Oral Supplements For Yeast Infection
Other Situations In Which The Diagnosis Of Acute Hiv Infection Is Made
There is increasing interest in not missing patients actively seroconverting to HIV. Since signs and symptoms may be absent or minimal, targeted screening of symptomatic patients is likely to miss a substantial number of people. Consequently, approaches have been considered to screen all antibody-negative individuals with a virologic test. In these settings, it is possible that patients will present for routine screening HIV antibody testing and be found seroconverting to HIV. The assays most frequently employed are:
Pooled HIV RNA testing: This involves taking the serum or plasma from those found to be HIV antibody negative on routine screening and pooling them. In this setting, a single HIV RNA assay can determine if HIV is present in any of the pooled samples. Further testing is performed to pinpoint which of the samples included in the pool was actually positive.
HIV antibody/p24 antigen combination assay: This is a standard enzyme-linked immunoassay that detects the presence of HIV antibody, p24 antigen, or both. If the test is positive, the patient can be further evaluated with an HIV antibody test and Western blot, which will define if the reactive result was from the presence of antibodies in a patient with chronic infection versus p24 antigen in an antibody-negative or indeterminate patient.
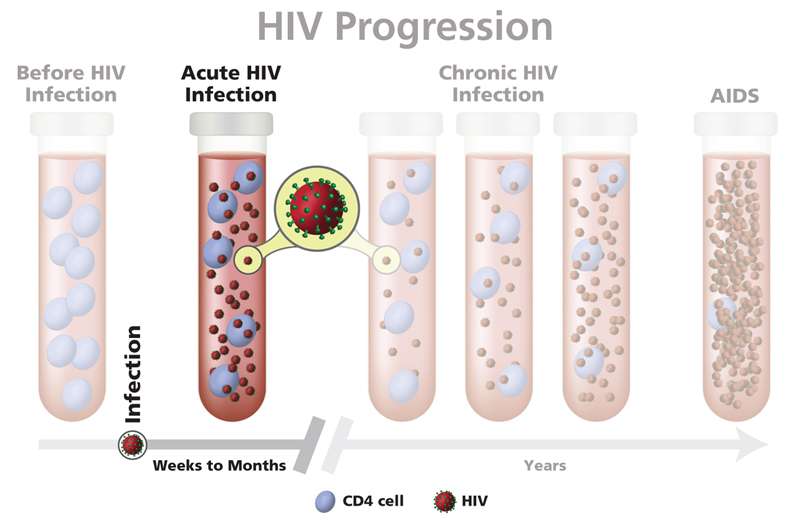
Stage : Clinical Latency
In this stage, the virus still multiplies, but at very low levels. People in this stage may not feel sick or have any symptoms. This stage is also called chronic HIV infection.
Without HIV treatment, people can stay in this stage for 10 or 15 years, but some move through this stage faster.
If you take HIV medicine exactly as prescribed and get and keep an undetectable viral load, you can live and long and healthy life and will not transmit HIV to your HIV-negative partners through sex.
But if your viral load is detectable, you can transmit HIV during this stage, even when you have no symptoms. Its important to see your health care provider regularly to get your viral load checked.
Read Also: What To Do If You Have A Wisdom Tooth Infection
What Happens After A Person Gets Hiv Infection
After acute HIV infection, your body works hard to attack the virus. With your body fighting, the virus can’t make so many virus pieces. Even though you still have HIV infection, you’ll begin to look well and feel well again. The usual blood tests will be normal.
However, during this time, the virus pieces are still attacking your lymph nodes. Lymph nodes are the centers of your body’s immune system. The virus may also attack your brain tissue and slowly cause damage there.
Over 10 to 15 years, HIV would kill so many CD4 cells that your body could no longer fight off infections. At this point, we would say that you have AIDS . Once you have AIDS, you can easily get many serious infections.
Does It Help Me To Find Out I Have Hiv At An Early Stage
Yes. Right now, we have no cure for HIV infection. Your body can make antibodies and killer T-cells to slow down the progress of HIV, but they can’t get rid of the virus. In fact, the very act of going after HIV may wear out your immune system in a short time.
However, we know that treatment with HIV medicines can hold down the virus and keep your body’s immune system strong for a longer time. That’s why the Centers for Disease Control and Prevention recommends early treatment of people with acute HIV syndrome.
Recommended Reading: Can A Tooth Infection Make Your Face Swell
Second Stage: Clinical Latency Symptoms
After your immune system loses the battle with HIV, the flu-like symptoms will go away. But thereâs a lot going on inside your body. Doctors call this the asymptomatic period or chronic HIV infection.
In your body, cells called CD4 T cells coordinate your immune systemâs response. During this stage, untreated HIV will kill CD4 cells and destroy your immune system. Your doctor can check how many of these cells you have with blood tests. Without treatment, the number of CD4 cells will drop, and youâll be more likely to get other infections.
Most people don’t have symptoms they can see or feel. You may not realize that you’re infected and can pass HIV on to others.
If youâre taking ART, you might stay in this phase for decades. You can pass the virus on to other people, but itâs extremely rare if you take your medicines.
Benefits And Risks Of Art
Benefits and Risks of ART
|
Antiretroviral therapy refers to the use of pharmacologic agents that have specific inhibitory effects on HIV replication. The use of fewer than three agents is not recommended for initiating rapid treatment. These agents belong to six distinct classes of drugs: the nucleoside and nucleotide reverse transcriptase inhibitors , the non-nucleoside reverse transcriptase inhibitors , the protease inhibitors , the fusion inhibitors , the CCR5 co-receptor antagonists, and the integrase strand transfer inhibitors . See all commercially available antiretroviral drugs that are approved by the U.S. Food and Drug Administration for the treatment of HIV/AIDS.
Don’t Miss: Need Antibiotics For Ear Infection
Getting Tested For Hiv
HIV testing is important. Someone living with HIV who isnt getting treatment can still transmit the virus, even if they have no symptoms. Others may pass the virus to others through an exchange of bodily fluids. But todays treatment can effectively eliminate the risk of transmitting the virus to a persons HIV-negative sexual partners.
According to the CDC , antiretroviral therapy can lead to viral suppression. When someone with HIV can maintain an undetectable viral load, they cant transmit HIV to others. The CDC defines an undetectable viral load as fewer than 200 copies per milliliter of blood.
Taking an HIV test is the only way to determine whether the virus is in the body. There are known risk factors that increase a persons chance of contracting HIV. For example, people whove had sex without a condom or shared needles may want to consider seeing their healthcare professional about getting tested.
Early Immune Response As Predictor Of Disease Progression
Investigators have shown that individuals have qualitatively different immune responses to primary HIV infection. Several research groups have shown that persons with strong initial CD8 T cell responses have lower HIV RNA levels after 6 to 12 months, and subsequently experience a slower progression of their HIV disease . More recently, the importance of the epitope-specific type of CD8 T cell response in controlling HIV has been elucidated. In most persons newly infected with HIV, higher initial HIV RNA levels predict an accelerated course of HIV disease progression, but this correlation is not universal. Similarly, several reports have suggested that development of clinically apparent acute retroviral syndrome portends a faster progression to AIDS. One study found that among 218 African women with HIV-1, a greater set point viral load or greater severity of acute HIV illness predicted faster progression to death .
Also Check: Over The Counter For Bv Infection
What Are The Clinical Features Of Acute Hiv Infection Syndrome
Acute HIV infection syndrome is classified according to general, neurologic, and dermatological manifestations.1 Fever is the most common symptom. None of the symptoms or signs of acute HIV infection syndrome are specific to acute HIV infection. 47 However, they are very infectious at this time due to the high HIV viral load. Early diagnosis is important to prevent sexual transmission during the highly viraemic phase of acute HIV infection.
What Laboratory Studies Should You Order And What Should You Expect To Find
The biggest challenge to making the diagnosis of acute HIV infection is thinking of it when a patient presents with any risk factors and a compatible clinical syndrome. This requires abandoning traditional stereotypes as to who is at risk so as to consider the diagnosis in all sexually active individuals and those potentially sharing needles. The second obstacle to making the diagnosis is recognizing that, during this stage of disease, patients are often HIV antibody negative with high levels of circulating virus . When acute HIV infection is considered in the differential diagnosis, the following tests should be performed:
Figure 2.
Timeline for the emergency of viral markers and antibodies during acute HIV infection
Combined screening tests: These tests detect both antibodies against HIV and the p24 antigen. A negative combined screening test is a strong argument against acute HIV infection. In rare cases, HIV-RNA may be present, whereas P24 antigen is still undetectable, so that a repeated combined screening test or a measurement of HIV-RNA may be indicated.
HIV virologic tests: Unlike the antibody test, which detects the humoral immune response to viral antigens, these tests identify circulating virus in the blood of infected patients. During acute infection, when antibodies are just emerging, the level of virus in blood often exceeds those seen in patients with the most advanced stages of chronic infection. Potential tests include:
Don’t Miss: How Do I Know If Eczema Is Infected