When Should I See A Doctor
A mild ear infection may go away on its own. But most cases of moderate to severe ear pain require a visit to your doctor. You should also see your doctor if youre experiencing ear discharge, fever, or chills.
Children with ear infections may constantly cry due to pain and discomfort. They might also tug or pull at the affected ear. See your doctor if symptoms dont improve within , or if they get worse.
Other signs that you should see a pediatrician include:
- fever of 102.2°F or higher
How Do You Prevent Ear Infections
You may be able to prevent ear some ear infections if you:
- Use earplugs when swimming or diving
- Dry ears thoroughly after swimming
- Never use cotton swabs inside the ear canal
- Wash hands properly to prevent the spread of viruses
- Use soap and warm water and wash for at least 20 seconds
What Research Is Being Done
The most important recent development to potentially reduce the frequency of ear infections is a new pneumococcal conjugate vaccine. A study from Northern California suggests that this vaccine could prevent about 7% of overall episodes of ear infections, and up to 23% of recurrent ear infections.
The new pneumococcal vaccine contains 7 of 90 types of pneumococcus, which are the most common and the most resistant bacteria. Elimination of these resistant types could have an impact on the number of antibiotic failures in children. This also could mean a reduction in the placement of tubes, possibly by one-fourth, as observed in the California study.
This vaccine is administered to infants at 2, 4, 6, and 12 months of age. Side effects have been minimal, and it has been a very safe vaccine. It uses the same technology as the universally administered HIB vaccine.
Some new antibiotics are about to undergo testing in children with acute otitis media. In preliminary testing, these drugs appear to work against the resistant pneumococcus.
About the Author
Dr. Block is a full-time practicing pediatrician in rural Bardstown, Kentucky who serves on the clinical faculties at both the University of Kentucky and the University of Louisville as an Associate Clinical Professor of Pediatrics.
His pediatric practice is one of the leading pediatric research groups in the United States and, in fact, Dr. Block was awarded the American Academy of Pediatrics 1998 Practitioner Research Award.
Recommended Reading: How To Avoid Hiv Infection
How Does It Cause Disease
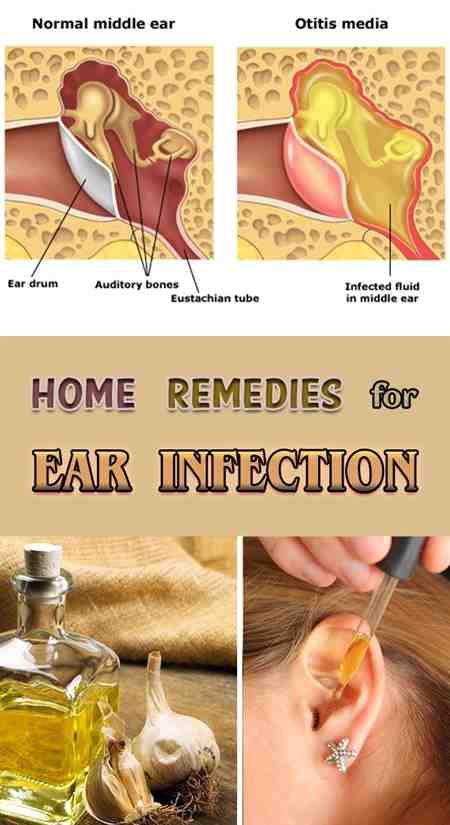
As long as air entering from the back of the nose is able to reach the middle ear space via the eustachian tube, the middle ear rarely becomes infected. The eustachian tube in younger children is flimsy and easily collapses. As the child grows, the cartilage tissue surrounding the eustachian tube becomes stiffer, longer, and more angulated inside the skull.
Pneumococcus, Haemophilus, and Moraxella commonly reside in the back of the nose, and do not infect the child. Once a child becomes infected with a respiratory virus, it not only causes congestion of the nose and the lungs, but also of the eustachian tube. When this tube becomes clogged, the cells in the middle ear space produce a fluid-like substance, which allows bacteria to grow and infect the middle ear space. A virus infection precedes up to 90% of cases of acute otitis media.
Respiratory virus infections also trigger ear infections by upsetting the body’s normal defenses in the nose and the eustachian tube, and allowing certain normal bacteria that reside in the nose to “stick” better to the lining of the nose and the eustachian tube. Certain viruses, such as the flu and RSV , are more frequently associated with ear infections. Occasionally, the child’s nose becomes colonized by a new aggressive strain of bacteria, which rapidly invades the middle ear. Unfortunately, more exposures to viruses and new strains of bacteria increase the likelihood of ear infections.
Infections Inside The Ear
Antibiotics are not usually offered because infections inside the ear often clear up on their own and antibiotics make little difference to symptoms, including pain.
Antibiotics might be prescribed if:
- an ear infection does not start to get better after 3 days
- you or your child has any fluid coming out of the ear
- you or your child has an illness that means there’s a risk of complications, such as cystic fibrosis
They may also be prescribed if your child is less than 2 years old and has an infection in both ears.
You May Like: Infected Sweat Gland Home Remedy
Can Ear Infections Affect Hearing
Fluid buildup in the middle ear also blocks sound, which can lead to temporary hearing problems. Kids having a problem might:
- not respond to soft sounds
- need to turn up the TV or radio
- talk louder
- seem inattentive at school
In kids who have otitis media with effusion, the fluid behind the eardrum can block sound, so mild temporary hearing loss can happen, but might not be obvious.
A child whose eardrum has ruptured might have ringing or buzzing in the ear and not hear as well as usual.
What Does The Eardrum Look Like When It Is Infected
When a doctor examines the eardrum through the otoscope instrument, the eardrum normally appears as a thin gray, translucent membrane . When infected, it will look opacified , very reddened, and yellowish. Sometimes, it shows a small layer of pus-like material. During an infection, the eardrum usually becomes rigid because of the accumulation of fluid, and it will not wiggle when the doctor puffs a small amount of air against the eardrum with an otoscope. Use of tympanometry or acoustic reflectometry may help to determine if there is fluid behind the eardrum. Neither instrument distinguishes between infected or uninfected fluid.
From the appearance of the eardrum, the doctor cannot determine the type of bacteria, or whether bacteria or viruses are causing the infection. The eardrum in children with otitis media with effusion appears as an orangish or dull, straw-colored fluid, and it also does not move when air is applied to it.
Recommended Reading: How To Diagnose Viral Infection
Risk Factors For Ear Infections
Ear infections occur most commonly in young children because they have short and narrow Eustachian tubes. About of children develop an acute ear infection at some point.
Infants who are bottle-fed also have a higher incidence of ear infections than their breastfed counterparts.
Other factors that increase the risk of developing an ear infection are:
- altitude changes
- Take OTC decongestants like pseudoephedrine .
- Avoid sleeping on the affected ear.
How Do Ear Infections Happen
A middle ear infection usually happens because of swelling in one or both of the eustachian tubes . The tubes let mucus drain from the middle ear into the throat.
A cold, throat infection, acid reflux, or allergies can make the eustachian tubes swell. This blocks the mucus from draining. Then, or grow in the mucus and make pus, which builds up in the middle ear.
When doctors refer to an ear infection, they usually mean otitis media rather than swimmer’s ear . Otitis media with effusion is when noninfected fluid builds up in the ear. It might not cause symptoms, but in some kids, the fluid creates a sensation of ear fullness or “popping.”
Don’t Miss: Oral Antibiotics For Kidney Infection
The Type Of Bacteria Involved
Bacteria are divided into two types depending on their external structure:
- Gram-positive bacteria which has thick, waxy external layer
- Gram-negative bacteria which has an extra lipid layer that acts as a barrier against certain antibiotics
When choosing an antibiotic, your healthcare provider first considers the type of bacteria involved. The type of bacteria can help determine which antibiotic drugs to choose, since not all antibiotics affect all bacteria.
How To Take Oral Antibiotics
Itâs important to always take your antibiotics as prescribed. It may be tempting to combine the doses, but they will not be as effective and could lead to adverse side effects, such as stomach upset.
Even if you begin to feel better, you should continue to take the antibiotics until you finish your medication to prevent the infection from returning. You should avoid alcohol while taking antibiotics.
While antibiotics are good for clearing a bacterial infection, they can also rid the body of helpful “good” bacteria at the same time. Because of this, you may want to consider taking a probiotic supplement while you are on antibiotics.
Probiotics are living organisms that can help to prevent the imbalance of bacteria within your gut that often comes from taking antibiotics. Studies have shown that taking probiotics while taking antibiotics can lower the chances of side effects from a bacterial imbalance, such as gastrointestinal upset and diarrhea.
Don’t Miss: Dr On Demand Tooth Infection
What Is The Treatment For Ear Infections
Medications used to treat ear infections include:
- Pseudoephedrine to ease ear pressure
- Antibiotic ear drops for infections of the ear canal
- Neomycin
- Polymyxin B
- Steroid ear drops for infections of the ear canal
- Hydrocortisone
- Oral antibiotics for infections of the middle ear , and severe infections of the outer ear
For mild cases of ear infection, doctors often recommend watching and waiting before starting use of antibiotics, as many cases will go away on their own. Consult your childs pediatrician before giving any over-the-counter medications to your child.
Home remedies to relieve symptoms include:
- Warm compresses applied to the area to help soothe pain
- Over-the-counter pain eardrops
What Is The Best Antibiotic For An Ear Infection
Looking for the best antibiotic for an ear infection. Antibiotics are recommended for a few kinds of bacterial ear infections in grown-ups. Since various kinds of ear diseases require diverse treatment, your specialist will complete a watchful examination and acquire your wellbeing history before choosing the best antibiotic for an ear infection.
If you need more information or you have a question regarding Ear Infection, you can discuss it with our HearingSol healthcare professionals, just give us a call on +91-9899437202. We are always here to help you.
When your child has an ear infection, there are a lot of questions that come to your mind because you are worried about your child. What are the precautions you should take? Which antibiotics are suitable for you? Read it you will find your way to get rid of your problems.
Don’t Miss: Can You Get Over A Yeast Infection Without Treatment
When To See Your Doctor
See your doctor if your child:
- Is six months of age or younger
- Has a high fever or bad earache
- Has an ear discharge that lasts more than 24 hours
- Continues to have fever or bad earache two days after they start treatment
- Still seems to have trouble hearing after six to eight weeks
- Seems to be getting worse or you are worried at any time.
Is An Ear Infection Contagious
To some degree, the bacteria that cause ear infections are contagious because they may colonize, or set up residence, in the nose of children or close contacts. However, only a small proportion of children colonized with a new strain of bacteria will develop an ear infection. For example, in the case of pneumococcus, only about 15% of children colonized in the nose with a new strain of it will develop an ear infection, and usually only within the first month. Also, some bacterial strains appear more aggressive than others and will directly invade the middle ear.
What may be even more important than new bacterial colonization is the spread of respiratory viruses, particularly among children in daycare and pre-schools. Respiratory viruses are very contagious in close quarters. They frequently make a child more susceptible to an ear infection by upsetting the normal balance between the child’s local nose immunity and the co-inhabitant bacteria. When the child’s defenses are down, or the eustachian tube becomes clogged, the bacteria tend to infect the middle ear.
Recommended Reading: How To Get Antibiotics For Tooth Infection
Watchful Waiting Makes Sense In Most Cases
In most children it’s best to wait for two to three days in order to see whether the symptoms improve on their own, and then decide whether to use . This can help avoid side effects. Painkillers will relieve the pain more quickly than antibiotics. If you take a “watchful waiting” approach, it’s a good idea to go to back to the doctor for a check-up.
Who Cannot Take Antibiotics
It is very rare for anyone not to be able to take some type of antibiotic. The main reason why you may not be able to take an antibiotic is if you have had an allergic reaction to an antibiotic in the past. Even if you have had an allergic reaction to one antibiotic, your doctor or health professional will be able to choose a different type of antibiotic, which you will be able to take. If you are pregnant, there are certain antibiotics you should not take, but your health professional will be able to advise on which one is suitable if an antibiotic is needed. If you are on some medication, certain antibiotics may need to be avoided, or your regular medication stopped whilst you take the antibiotic. As above, when prescribed an antibiotic, make sure the prescriber knows about any other medication you take.
How to use the Yellow Card Scheme
If you think you have had a side-effect to one of your medicines you can report this on the Yellow Card Scheme. You can do this online at www.mhra.gov.uk/yellowcard.
The Yellow Card Scheme is used to make pharmacists, doctors and nurses aware of any new side-effects that medicines or any other healthcare products may have caused. If you wish to report a side-effect, you will need to provide basic information about:
- The side-effect.
- The name of the medicine which you think caused it.
- The person who had the side-effect.
- Your contact details as the reporter of the side-effect.
Don’t Miss: What Is A Tooth Infection Called
When Else Are Antibiotics Needed
Antibiotics can be the right treatment for kids who get a lot of ear infections. Their doctors might prescribe daily antibiotics to help prevent future infections. And younger children or those with more severe illness may need antibiotics right from the start.
The “wait-and-see” approach also might not apply to children with other concerns, such as cleft palate, genetic conditions such as Down syndrome, or other illnesses such as immune system disorders.
Antibiotics For Ear Infections
Amoxicillin is one of the most commonly prescribed antibiotics to get rid of ear infections. In case, amoxicillin doesn’t work, a stronger antibiotic such as Augmentin ES may be recommended.
Amoxicillin is one of the most commonly prescribed antibiotics to get rid of ear infections. In case, amoxicillin doesnt work, a stronger antibiotic such as Augmentin ES may be recommended.
Ear infections are a result of bacteria making their way into the ear canal. However, bacteria can also gain access to ear parts by entering through the nose. Ear pain, runny nose, and partial blockage of ear due to formation of pus are some of the common symptoms of an ear infection, that can always be treated with antibiotics.
You May Like: Will Tooth Infection Go Away On Its Own
When Is Treatment With Antibiotics Necessary For An Ear Infection
If your child is in a lot of pain, and the symptoms last more than a few days, your pediatrician will likely recommend a round of antibiotics. According to the AAFP, here are some of the circumstances where antibiotics are likely to be prescribed for an ear infection:
- Infants six months or younger.
- Babies ages six months to two years, who have moderate to severe ear pain.
- Children 2 years or older who have a fever of 102.2 or higher.
- Children with another condition that could make an infection harder to heal, including cleft palate, Down syndrome, immune disorders and cochlear implants.
Who Gets An Ear Infection
![7 Home Remedies For Ear Infections! [2021 UPDATED!] 7 Home Remedies For Ear Infections! [2021 UPDATED!]](https://www.infectiontalk.net/wp-content/uploads/7-home-remedies-for-ear-infections-2021-updated.jpeg)
At the highest risk for ear infections include those children who:
- Are male
- Have a strong family history of otitis media
- Were not breastfed during the first 12 months of life and/or
- Reside in a smoking household.
Children with a cleft palate or HIV have particularly severe problems with recurrent ear infections.
Age affects the rate of acute otitis media, with a dramatic decline in frequency in children older than three years. However, some children with a history of ventilating tubes or frequent recurrent otitis media, severe allergies, or large adenoids may still be plagued with ear problems.
Don’t Miss: What Do Doctors Prescribe For Yeast Infections
Diagnosis Of Ear Infections
Your physician will look into your ear with an otoscope, a medical instrument with a light on one end designed to get a better view inside the ear. Your doctor will look for the visual signs of ear infection, such as redness and inflammation.
To check for fluid buildup, a pneumatic otoscope, which blows air at the eardrum, will be used. If there is excessive fluid behind the eardrum, it will not move as it should when the air hits it.
In some cases, hearing tests may also be performed to assess any damage to the ear from the infection.
Different types of ear infections present with different symptoms, which can include:
- Inner ear infections: Hearing loss, ringing in the ears , dizziness, loss of balance, nausea and vomiting, and ear pain
- Middle ear infections: Fluid in the ear, ear pain, fever, a feeling of general illness, pressure in the ears, and hearing loss
- Outer ear infections: Inflammation of the ear canal, itching in the ear, ear pain, swelling of the ear canal, redness, and fluid draining from the ear
Ear Infection Doctor Discussion Guide
Children with ear infections, especially toddlers or infants, may not be able to describe their symptoms, but an ear infection will often present with the following signs:
- Tugging or pulling at their ears
- Fussing or crying
- Being clumsy and having balance issues
- Trouble hearing or responding to quiet noises