Safe Management Of Blood And Body Fluids
Healthcare facilities must ensure all staff is correctly trained on the decontamination of spillages of blood or other bodily fluids.
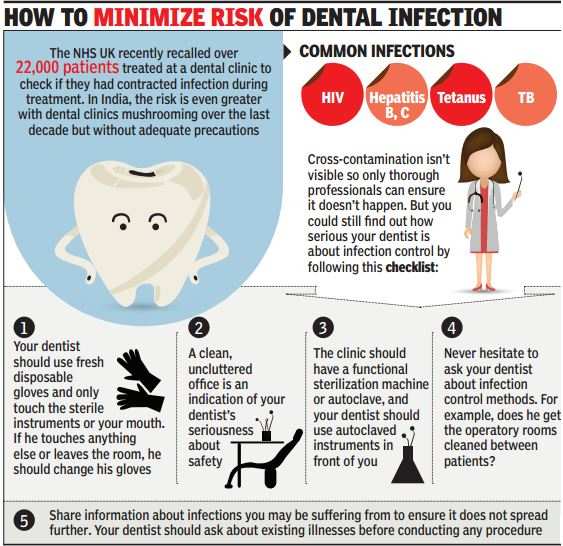
These spillages may transmit blood-borne viruses such as Hepatitis or HIV, therefore they must be dealt with swiftly.
The responsibilities for the decontamination for spillages of blood or body fluids will be clear within each setting. It is recommended to ensure easy access to a blood or body fluid spillage kit.
Respiratory Hygiene And Etiquette
- Everyone needs to watch for and report respiratory illness.
- Vaccinations are an important tool for preventing respiratory illnesses such as influenza and pneumococcal pneumonia.
- Staff should stay home if they are sick.
- Staff should go home if they develop respiratory symptoms while working.
- A virus can cause a cold for a staff member but may develop into a serious illness for an older adult.
- Visitors, families, and staff can be a source of respiratory illness outbreaks.
- Cover coughs, and wear a mask if recovering from an illness.
- Educate residents and visitors to cover their mouths and noses with a tissue when coughing or sneezing.
- Residents should stay in their rooms if they develop a new cough with fever or other symptoms of a respiratory infection.
Basic Background
Respiratory illnesses, including pneumonia, are a major cause of outbreaks in LTC facilities. While a virus can cause a cold for a staff member, it can develop into a serious illness for an older adult. Respiratory illnesses often result in hospital staysâand sometimes even death.
Practice Tips
- Pay attention to coughing and sneezing residents, family members, visitors, and staff.
- Always cover your mouth and nose with your sleeve or a tissue when coughing or sneezing and then perform hand hygiene.
- Make sure infected residents wear a mask whenever they leave their rooms.
Communication Tips
Director Of Public Health
The Director of Public Health is accountable for the delivery of their local authoritys public health duties, and is a statutory chief officer of their authority. The role is wide ranging, and has both statutory and non-statutory responsibilities.
The Director of Public Health provides advice and expertise to the local authority and public on a range of health issues, from outbreaks of disease and emergency preparedness through to improving the health of local populations.
Don’t Miss: Have Uti Symptoms But No Infection
Respiratory And Cough Hygiene
Proper respiratory and cough hygiene practices aim to reduce the risk of cross-transmission of different respiratory illnesses and pathogens such as, influenzas or COVID-19.
- Cover nose and mouth with disposable tissues if coughing or blowing/wiping the nose
- Bin the tissue after use
- Ensure you wash your hands after
Healthcare professionals should both practice respiratory and cough hygiene themselves and encourage it among patients. Ensure there are tissues, plastic bags for the used tissues and handwashing stations.
Using Aseptic Technique At Home
The proper execution of aseptic technique requires training. If a person needs to use aseptic technique at home, a trained healthcare professional can demonstrate the proper practices to them.
Anyone performing aseptic techniques at home will need to have sterile gloves and special dressing kits at hand.
While aseptic technique requires proper training and the use of specialist equipment, clean technique is much easier to achieve at home. Clean technique involves thoroughly washing the hands, wearing gloves, and maintaining a clean environment.
Don’t Miss: Where Do I Go For A Yeast Infection
Appendix : Glossary Of Terms
Antimicrobial: a drug that selectively destroys or inhibits the growth of microorganisms. Sometimes referred to as an antimicrobial agent. Examples include antibiotics antiviral and antifungal agents.
Antibiotic resistant bacteria: bacteria with the ability to resist the effects of an antibiotic to which they were once sensitive.
Antimicrobial resistance : occurs when the microorganisms that cause disease cease to be affected by the drugs we use to kill them and treat the disease.
Cleaning: a process that physically removes contamination but does not necessarily destroy micro-organisms.
Disinfection: a process used to reduce the number of viable micro-organisms, but which may not necessarily inactivate some bacterial agents, such as certain viruses and bacterial spores.
Alcohol-based handrub: a preparation applied to the hands to reduce the number of viable microorganisms. This guideline refers to handrubs compliant with British standards .
Impermeable bag: bags that a liquid does not leak or pass through at any time during their use or during the washing process.
Pathogen or pathogenic: an infectious agent , a microorganism such as a virus, bacterium, or fungus that causes disease in its host.
Personal protective equipment : equipment that is intended to be worn or held by a person to protect them from risks to their health and safety while at work. Examples include gloves, aprons and eye and face protection.
Water-soluble bags are:
Food Preparation And Workplace Infection Control
When preparing food:
- Wash your hands before and after handling food.
- Avoid touching your hair, nose or mouth.
- Keep hot food hot and cold food cold.
- Use separate storage, utensils and preparation surfaces for cooked and uncooked foods.
- Wash all utensils and preparation surfaces thoroughly with hot water and detergent after use.
Also Check: Where To Go For Kidney Infection
Uk Health Security Agency
UKHSA is responsible for protecting every member of every community from the impact of infectious disease, and providing intellectual, scientific and operational leadership at national and local level, as well as on the global stage, to make the nations health secure. Local health protection teams provide specialist public health advice and operational support.
Invasive Devices And Wounds
People with non-intact skin or an invasive device are at increased risk of infection.
Evidence-based clinical guidelines for wound management and management of invasive devices should be followed. Specific training to ensure competency is needed for those supporting people with invasive devices or wounds.
People and their family members or carers should be supported in understanding and applying safe management of invasive devices or equipment, including techniques to prevent infection where this is appropriate to do so.
Accurate and complete records should be kept regarding the care and maintenance of any device.
Manufacturers instructions for use, storage and changing intervals must be followed.
The NICE guidance on healthcare-associated infections: prevention and control in primary and community care provides further useful information on long-term urinary catheters, enteral feeding and vascular access devices.
Also Check: Otc Urinary Tract Infection Medication
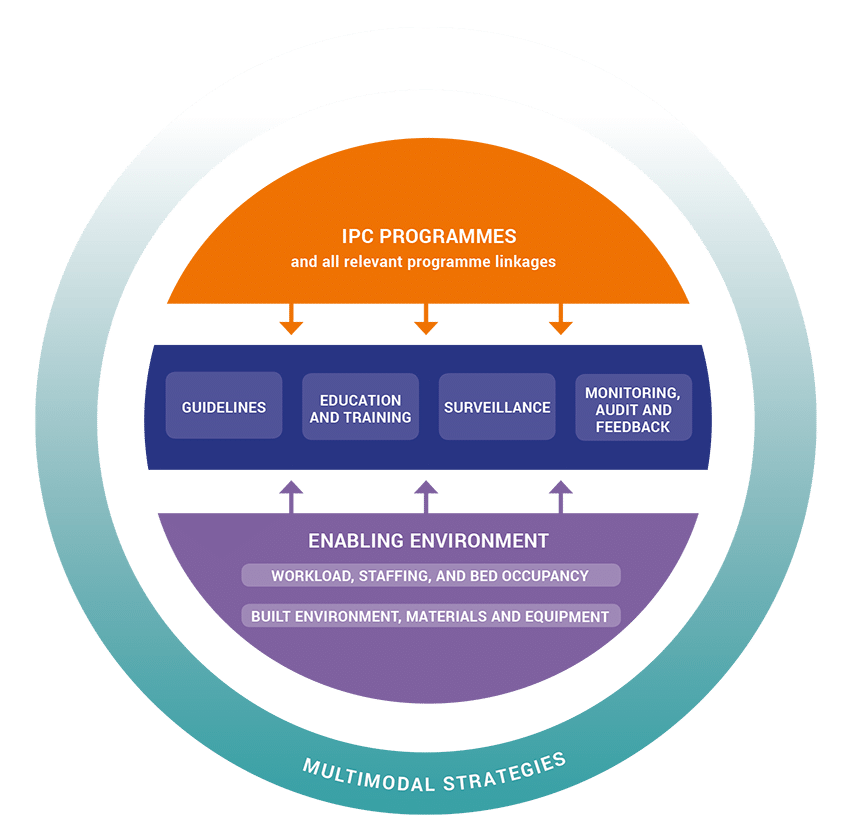
Infection Prevention And Control
Infection prevention and control is a practical, evidence-based approach preventing patients and health workers from being harmed by avoidable infections. Effective IPC requires constant action at all levels of the health system, including policymakers, facility managers, health workers and those who access health services. IPC is unique in the field of patient safety and quality of care, as it is universally relevant to every health worker and patient, at every health care interaction. Defective IPC causes harm and can kill. Without effective IPC it is impossible to achieve quality health care delivery.
Infection prevention and control effects all aspects of health care, including hand hygiene, surgical site infections, injection safety, antimicrobial resistance and how hospitals operate during and outside of emergencies. Programmes to support IPC are particularly important in low- and middle-income countries, where health care delivery and medical hygiene standards may be negatively affected by secondary infections.
The first WHO Global Patient Challenge laid the foundations for the IPC Global Unit, which works to support country capacity-building for IPC action. Through this programme, WHO provides technical assistance for developing local IPC policies and guidelines, performs in-country assessments, convenes meetings focused on guideline development and provides ongoing support for health care providers.
Controlling Infectious Diseases Within Communities
Infection control and prevention is a global issue and there are many protocols and guidelines that can be followed to minimise the spread of infection between people, within a population and globally. Identifying at-risk groups such as children, older people and those with chronic conditions can also help guide relevant strategies to protect these vulnerable groups. The first step when looking at infection control can start at the community level by changing behaviour, including:
Recommended Reading: Urinary Tract Infection How To Treat Without Antibiotics
Infection Control Programmes Globally
The WHO Guidelines on the Core Components of IPC Programmes at the national and facility level aim to enhance the capacity of countries to develop and implement effective technical and behaviour modifying interventions. They form a key part of WHO strategies to prevent current and future threats from infectious diseases such as Ebola, strengthen health service resilience, help combat antimicrobial resistance and improve the overall quality of health care delivery. They are also intended to support countries in the development of their own national protocols for IPC and AMR action plans and to support health care facilities as they develop or strengthen their own approaches to IPC.
The “Executive Summary of the Minimum Requirements by Core Component” provides a good summary to present and promote the minimum requirements for IPC programmes at the national and health care facility level, identified by expert consensus according to available evidence and in the context of the WHO core components.
The Purpose Of Infection Control Procedures Is To A
- Ratings91%32 out of 35 people found this document helpful
Course Hero uses AI to attempt to automatically extract content from documents to surface to you and others so you can study better, e.g., in search results, to enrich docs, and more. This preview shows page 7 – 9 out of 11 pages.
Upload your study docs or become a
Course Hero member to access this document
Read Also: Numbing Ear Drops For Ear Infection
Routine Practices And Additional Precautions
Infection prevention and control best practices used by health care workers can reduce the risk of transmitting infections to and from clients, patients, residents and staff in all health care settings. Routine practices refer to minimum practices that should be used with all clients, patients or residents. Additional precautions refer to specific actions that should be taken with individuals that are at risk of transmitting or acquiring disease. We offer expertise, best practices and resources to help you understand and apply routine practices and additional precautions.
Environmental Infection Prevention And Control
Policies and procedures for routine cleaning and disinfection of environmental surfaces should be included as part of the infection prevention plan. Cleaning removes large numbers of microorganisms from surfaces and should always precede disinfection. Disinfection is generally a less lethal process of microbial inactivation that eliminates virtually all recognized pathogenic microorganisms but not necessarily all microbial forms .
Additional guidance for the cleaning and disinfection of environmental surfacesincluding for cleaning blood or body substance spillsis available in the Guidelines for Environmental Infection Control in Health-Care Facilities and the Guideline for Disinfection and Sterilization in Healthcare Facilities .
a. Use surface barriers to protect clinical contact surfaces, particularly those that are difficult to clean and change surface barriers between patients.
b. Clean and disinfect clinical contact surfaces that are not barrier-protected with an EPA-registered hospital disinfectant after each patient. Use an intermediate-level disinfectant if visibly contaminated with blood.
Recommended Reading: Should Physicians Prescribe Antibiotics For Viral Infections
Workplace Infection Control Personal Hygiene Practices
Infection control procedures relating to good personal hygiene include:
- hand washing the spread of many pathogens can be prevented with regular hand washing. Thoroughly wash your hands with water and soap for at least 15 seconds after visiting the toilet, before preparing food, and after touching clients or equipment. Dry your hands with disposable paper towels
- unbroken skin intact and healthy skin is a major barrier to pathogens. Cover any cuts or abrasions with a waterproof dressing
- gloves wear gloves if you are handling body fluids or equipment containing body fluids, if you are touching someone else’s broken skin or mucus membrane, or performing any other invasive procedure. Wash your hands between each client and use fresh gloves for each client where necessary
- personal items don’t share towels, clothing, razors, toothbrushes, shavers or other personal items.
Infection Prevention And Control: Resource For Adult Social Care
This publication is licensed under the terms of the Open Government Licence v3.0 except where otherwise stated. To view this licence, visit nationalarchives.gov.uk/doc/open-government-licence/version/3 or write to the Information Policy Team, The National Archives, Kew, London TW9 4DU, or email: .
Where we have identified any third party copyright information you will need to obtain permission from the copyright holders concerned.
This publication is available at https://www.gov.uk/government/publications/infection-prevention-and-control-in-adult-social-care-settings/infection-prevention-and-control-resource-for-adult-social-care
This guidance applies from 4 April 2022.
Read Also: What Does A Sinus Infection Smell Like
Safe Management And Care Of Environment
The environment for patients and healthcare staff must be safe for practice. Even if an area may look clean many dangerous micro-organisms can live on surfaces. There are many hotspots for these pathogens to live such as door handles, rails, tables, etc.
Therefore, the cleaning of these high-risk touchpoints is essential. When cleaning it is essential the appropriate cleaning products and disinfectants are used. Healthcare professionals should be aware of the schedules and responsibilities for cleaning and disinfecting the area and every facility should have strict cleaning protocols.
Environmental Cleaning And Disinfection
- Personal care wipe packages
When cleaning, consider the contact time for the product. Contact time is the length of time a disinfectant needs to remain wet on a surface to be effective.
Practice Tips
- Wear gloves if the cleaning product requires them.
- Change gloves between rooms and when moving from a contaminated surface area to a clean one.
- Use the right product for the right surface.
- Make sure the product you are using stays wet on the surface for the time needed to kill germs.
- Do not flush wipes down the toilet.
- Do not mix chemicals as some combinations can release toxic gas.
- Keep chemicals locked up away from residents when not in use.
Communication Tips
- Ask the facility for training on how to use cleaning chemicals properly, and choose a surface-appropriate product.
- Suggest that the facility purchase wipes that are premoistened with cleaner/disinfectant as these are easier to use.
- Ask your supervisor how to alert residents and family members to use alcohol-based hand wipes to help keep their own rooms clean.
Also Check: Medicine For E Coli Infection
Dealing With Spills Of Body Fluids
Examples of body fluids include blood, saliva, urine and faeces. When dealing with spills of body fluids, infection control procedures need to be followed carefully. Always:
- Isolate the area.
- Wear gloves, a plastic apron and eye protection, such as goggles.
- Soak up the fluid with disposable paper towels, or cover the spill with a granular chlorine-releasing agent for a minimum of 10 minutes. Scoop up granules and waste using a piece of cardboard , place in a plastic bag and dispose of appropriately.
- Mix one part bleach to 10 parts water and apply to the area for 10 minutes.
- Wash the area with hot water and detergent.
- Dispose of paper towelling and gloves appropriately.
- Wash your hands.
- Rinse any contaminated clothing in cold running water, soak in bleach solution for half an hour, then wash separately from other clothing or linen with hot water and detergent.
Infection Control In Disaster And Conflict Settings
The principles of IPC remain of paramount importance in emergency settings in order to protect yourself and your patients. This is especially important given the unsanitary conditions post-disaster and conflict in camps, which can create a perfect storm for infection, both for infectious diseases and wound infection. With a high incidence of complex, open traumatic injuries requiring surgery performed in sub-optimal surgical environments, there comes an increased risk of wound infection, which is further exacerbated by limited access to resources including clear water and medical consumables, creating significant challenges for rehabilitation professionals in many disaster and conflict settings.
When working in an area where infectious diseases ) are an identified risk, additional IPC precautions will be in place. Make sure that you have had specific training and have been provided with additional PPE as required.
Also Check: Keep Getting Utis And Yeast Infections
Aseptic Technique Vs Clean Technique
Keeping the environment as clean as possible is always important in preventing infections. However, some situations call for aseptic technique while others call for clean techniques.
Healthcare providers learn both aseptic and clean techniques as part of their training. The goal of the aseptic technique is to eliminate germs entirely. The goal of the clean technique is to reduce the number of germs whenever possible. Clean techniques are important for all healthcare providers and their patients because they prevent infections every day.
Examples of clean techniques include washing hands and putting on clean gloves when needed. Healthcare providers keep a patients surroundings as clean as possible, but they arent using sterile items or aseptic technique.
Healthcare professionals commonly use clean techniques when theyre:
- giving an injection
- emptying a urinary catheter drainage bag
- giving a bed bath
- inserting a peripheral IV
- removing a peripheral IV
The Provincial Infectious Diseases Advisory Committee On Infection Prevention And Control
PIDAC-IPC is a multidisciplinary committee of health care professionals with expertise and experience in infection prevention and control. The committee advises PHO on the prevention and control of health care-associated infections, considering the entire health care system for the protection of clients/patients/residents and health care providers.
Also Check: Osha Hipaa And Infection Control Training
Infection Control Principles And Practices For Local Health Agencies
Standard Precautions
Standard precautions are a set of infection control practices used to prevent transmission of diseases that can be acquired by contact with blood, body fluids, non-intact skin , and mucous membranes. These measures are to be used when providing care to all individuals, whether or not they appear infectious or symptomatic.
Hand Hygiene
Hand hygiene refers to both washing with plain or anti-bacterial soap and water and to the use of alcohol gel to decontaminate hands. When hands are not visibly soiled, alcohol gel is the preferred method of hand hygiene when providing health care to clients.
Hand hygiene should be performed before and after contact with a client, immediately after touching blood, body fluids, non-intact skin, mucous membranes, or contaminated items , immediately after removing gloves, when moving from contaminated body sites to clean body sites during client care, after touching objects and medical equipment in the immediate client-care vicinity, before eating, after using the restroom, and after coughing or sneezing into a tissue as part of respiratory hygiene.
Observational auditing of appropriate hand hygiene by staff is essential for providing real-time feedback and education. An example tool for tracking hand hygiene audits in long-term care is available for use or adaptation.
Personal Protective Equipment
Needlestick and Sharps Injury Prevention
Cleaning and Disinfection
Respiratory Hygiene
Waste Disposal
Safe Injection Practices