How Often Should An Infection Control Audit Be Completed
The frequency of an infection control audit depends on the needs, current situation, and context of the healthcare institution. Generally, the International Federation of Infection Control affirms that an infection control audit should take place over a defined time using a rapid audit cycle plan or an overall annual plan.
For example, each specific area of an organization such as hand hygiene, indwelling lines, and urinary catheters, should be audited one day at a time and in an alternating pattern. Having audited each area twice with a 2-day interval, the infection control team will have results about the effectiveness of their safety measures within a week.
To provide a clearer picture of a sample infection control audit schedule, refer to the table below:
Proactive Icars: What To Expect
- The facility requests an assessment by completing the request form. If you would like to request an ICAR for more than one type of setting, please complete a request form for each setting.
- The facility will identify a primary point of contact for the visit
- Work with the VDH ICAR team over phone and/or email to schedule the site visit.
- The VDH ICAR team will send the facility a report with recommendations and resources.
- The recommendations report will summarize infection prevention strengths, areas of opportunity, and provide resources.
- The Infection Prevention Scoring Tool will also be shared, serving as a high-level summary of performance in each infection control category.
- Please check the Definitions section for more information on the scoring tool.
Environment Of Care And Cleaning Procedures
Your physical environment, plus your cleaning, disinfection, and sterilization practices, will also shape your IPC program. For example, many newer facilities incorporate evidence-based design to support and enhance infection control outcomes. Additionally, your level of investment in practices like antimicrobial stewardship will have a direct impact on your risk assessment.
Read Also: Middle Ear Infection Over The Counter
Tools For Healthcare Settings
The following tools are designed to help healthcare providers to implement Standard and Transmission-Based Precautions to prevent infections.
For more information, see the Infection Control Assessment Tool page on the HAI website.
The TAP strategy is a method developed by the CDC to use data for action to prevent healthcare-associated infections. The TAP strategy targets healthcare facilities and specific units within facilities with a disproportionate burden of HAIs so that gaps in infection can be addressed.
For more information on the TAP strategy and for prevention tools, see the Targeted Assessment for Prevention Strategy page on the HAI website.
Ambulatory/Outpatient Settings
- See Prevention Tools on the Long-Term Care facilities website.
Orthopedic and Pain Management Office Settings
- See Audit Tools and Checklists on the Dialysis Safety Website
Outpatient Oncology Settings
Immunizations
To receive email updates about this page, enter your email address:
Links with this icon indicate that you are leaving the CDC website.
CDC.gov Privacy Settings
We take your privacy seriously. You can review and change the way we collect information below.
Cookies used to make website functionality more relevant to you. These cookies perform functions like remembering presentation options or choices and, in some cases, delivery of web content that based on self-identified area of interests.
What Are The Five Basic Principles For Infection Control
Infection control audits cover all possible sources of infection in healthcare facilities with particular focus on the following :
Infection control program
The healthcare facility should have written infection control policies and procedures. Healthcare staff, as well as patients and their caregivers, should be empowered with training and knowledge on infection control.Special circumstances also call for strict compliance with measures implemented to prevent fast-spreading diseases from taking place in healthcare facilities.
Hygiene practices
Competency on proper hand hygiene is a must, particularly for healthcare providers. Routine monitoring of hand hygiene practices through internal audits can help ensure that proper hand hygiene is being practiced.
Personal Protective Equipment
One way to protect healthcare professionals from infection is through the proper use of PPE, which is standard procedure in any job that involves health risks.
Facility and equipment
Healthcare professionals should be knowledgeable in the use of ventilators and other hospital equipment. The proper disinfection of tools and equipment and the cleanliness of the healthcare facility must be maintained at all times.
Healthcare practice
Proper insertion and maintenance of catheters, injection practices, and other medical services must be done in adherence to the infection control protocols of the facility.
Recommended Reading: Retreating A Root Canal With Infection
Infection Control Assessment And Response
Health department staff conduct proactive infection prevention and control assessments at healthcare facilities that are not experiencing an outbreak. The assessments are not regulatory and are designed to identify a facilitys IPC program strengths and areas for opportunity.
During these onsite visits, health department staff assist healthcare facilities in reviewing current infection prevention practices and provide recommendations for improvement. The proactive assessments are conducted using a standardized set of infection control assessment and response tools developed by the Centers for Disease Control and Prevention. These tools may also be used by healthcare facilities as self-assessments to conduct internal quality improvement even after the visit.
Ashe Publishes Revised Infection Control Risk Assessment Guide
The ICRA 2.0 includes several improvements and clarifications to help in prevention planning for construction projects
The use of ICRAs during health care facility design and construction projects has been evolving for several decades.
Image by Getty Images
The use of infection control risk assessments during hospital design and construction projects has been evolving for the past several decades, according to the publication Using the Health Care Physical Environment to Prevent and Control Infection, published by the American Society for Health Care Engineering and other professional groups and associations in cooperation with the Centers for Disease Control and Prevention .
The first formal ICRA was introduced in the 1996 edition of the Facility Guidelines Institutes Guidelines for Design and Construction of Hospital and Healthcare Facilities, although earlier editions required construction and renovation assessments related to specific risks. The goal of the assessment was to describe how an organization determines the risk for transmission of various infectious pathogens through a multidisciplinary committee.
A subsequent effort was undertaken by ASHE with other organizations and experts in the field to clearly spell out what would be included in the ICRA process. In 2020, ASHE assembled another group of experts to update these guidelines, which is being called ICRA 2.0.
Also Check: Is Aleve Good For Tooth Infection
What Is An Infection Control Risk Assessment
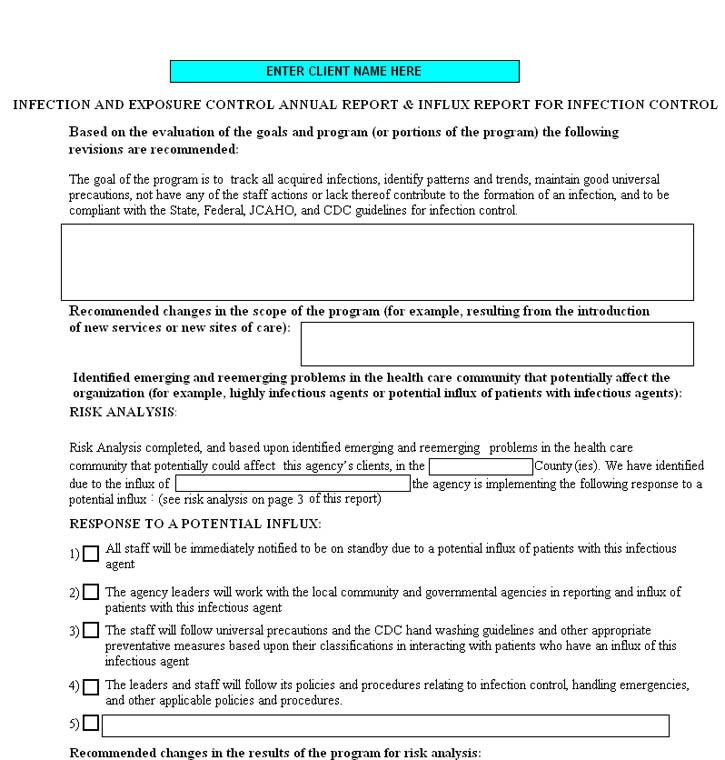
An infection control risk assessment is the process of preventing the spread of a highly contagious and infectious disease in the workplace, especially in the healthcare setting.
It is required that all offices and facilities should have an infection control policy in place. However, the infection control audit is different from industry to industry.
An infection control risk assessment is more than just documenting or informing authorities of the potential hazards. It serves as the foundation of an active infection and control prevention program. The guide evolves as goals and objectives change, but the framework remains solid to ensure the safety of the people in that area.
Infection Control Assessment Tools
ICAR: Infection Control Assessment and Response Program
IP: Infection Prevention
Healthcare Personnel IP Competency: The proven ability to apply essential knowledge, skills, and abilities to prevent the transmission of pathogens during the provision of care.
Healthcare Personnel IP Competency-Based Training: The provision of job-specific education, training, and assessment to ensure that healthcare personnel possess IP competency.
Competency Assessment: The verification of IP competency through the use of knowledge-based testing and direct observation. If direct observation is not included as part of a competency assessment, an alternative method to ensure that healthcare personnel possess essential knowledge, skills, and abilities should be used.
Audit: Direct observation or monitoring of healthcare personnel adherence to job-specific IP measures.
Feedback: A summary of audit findings that is used to target performance improvement.
The basic elements of an infection prevention program are designed to prevent the spread of infection in healthcare settings. When these elements are present and practiced consistently, the risk of infection among patients and healthcare personnel is reduced.
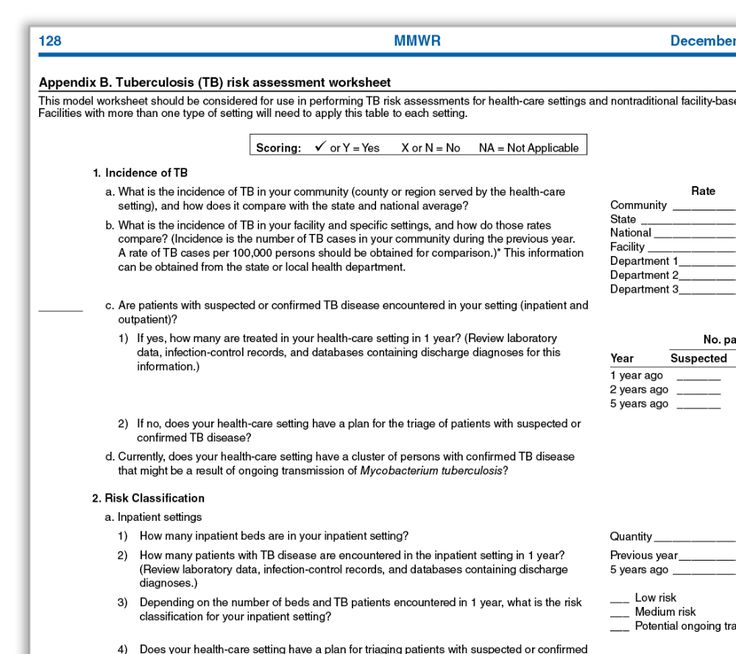
The Infection Control Assessment Tools were developed by CDC to assist health departments in assessing infection prevention practices and guide quality improvement activities . These tools may also be used by healthcare facilities to conduct internal quality improvement audits.
You May Like: Otc Oral Yeast Infection Medication
Reactive Infection Prevention & Control Assessments
Infection prevention and control assessments can also be conducted in response to an outbreak or known infection prevention concern. This type of assessment is called a reactive IPC assessment or reactive ICAR. The VDH HAI/AR Program recommends that a reactive ICAR be conducted when there has been an infection control breach or in response to certain types of outbreaks . Reactive assessments may include COVID-19 ICARs as well, which can be done via an onsite visit or virtually in certain circumstances. For questions regarding reactive ICARs and/or teleICARs, please contact .
Additional questions about ICARs? Please contact .
Elements To Consider When Conducting An Infection Risk Assessment
Almost everything we do in the healthcare industry is designed around one main focal point: patient safety. And infection prevention and control is no exception. Industry leaders are developing IPC protocols to keep patient safety and outcomes at the forefront of all decision making. That is why it is so important to take a proactive approach to preventing infections from occurring by assessing the risks that may derail IPC efforts.
Almost everything we do in the healthcare industry is designed around one main focal point: patient safety. And infection prevention and control is no exception. Industry leaders are developing IPC protocols to keep patient safety and outcomes at the forefront of all decision making. That is why it is so important to take a proactive approach to preventing infections from occurring by assessing the risks that may derail IPC efforts.
What is Infection Control Risk Assessment?An infection control risk assessment is more than just running down a list of potential hazards and informing personnel of best practices. A sophisticated infection control risk assessment is a living document that forms the foundation of any comprehensive IPC program. The policy evolves over time as goals and measurable objectives change, while maintaining a solid framework for consistent patient safety.
To understand which risks pose the greatest threats to your facility, you must assess your current operations.
You May Like: Vagisil Wipes For Yeast Infection
Proactive Onsite Infection Prevention & Control Assessments With Vdh
|
Optimize Your Healthcare Facility’s Infection Prevention and Control Program |
Eligibility
All Virginia acute and long-term acute care hospitals, long-term care facilities, outpatient clinics, and outpatient dialysis facilities are eligible to request proactive onsite IPC assessments.
Requirements
Completion of an ICAR assessment and site visit, along with a facility commitment to take measures to implement VDH recommendations to improve infection prevention and control practices.
Benefits to Participation
- Enhance your facilitys IPC capacity
- Receive free resources and recommendations to address IPC areas identified for improvement
- Strengthen the collaborative relationship between your healthcare facility and VDH
Why Conduct An Infection Control Risk Assessment
Risk assessments allow organizations to detect the presence of infection before it becomes present or severe. It can be easily stopped through early detection, minimize contamination, and eliminate its threat to the body.
Here are other benefits of having an infection control risk assessment:
Don’t Miss: Life Span Of Hiv Infected Person
Measurable: Make Use Of Data
The data you collect from clinical surveillance is one of the most powerful tools you have in infection control risk assessment. For example, if your antibiogram reveals increased resistance patterns for commonly seen organisms, your assessment should address this discovery. One highly useful tool in assessing program effectiveness is the CDCs Targeted Assessment for Prevention Strategy . TAP is a quality improvement framework that works by:
- Supporting hospital-acquired infection prevention and reduction
- Targeting locations with excess HAIs and implementing interventions
- Identifying gaps in prevention and opportunities for improvement, which serve as real-time teaching moments for multidisciplinary staff
However, manually aggregating data from disparate sources such as antibiograms and TAP can be a daunting and time-consuming task. All this information can be streamlined through use of an electronic clinical surveillance solution. While your staff focus on consultation and education, clinical surveillance can:
- Automatically identify potential or actual HAIs
- Aggregate and analyze infection prevention data
- Streamline daily surveillance workflows
Budgeting your time for analysis and patient care is critical in the face of the ongoing COVID-19 pandemic.
Timely: Assess Infection Prevention Programs Annually
Your risk assessments should be performed annually, and possibly more frequently if your findings warrant it. Ongoing review is critical to IPC program success. Regular check-ins help you identify high-risk patients early, reduce the incidence of HAIs and strengthen your antimicrobial stewardship practices to improve patient care and safety. Your teams multidisciplinary approach combined with the right technology and metrics will make your IPC program more effective and efficient, benefiting patients, visitors, staff and your entire care community.To get ahead of scheduling difficulties, consider the following best practices curated by our experienced infection prevention team:
- Dont push the date past its deadline.
- Begin assessment earlier than the deadline to avoid citation for lateness.
- Note events during the year that might significantly affect your assessment and that could trigger a revision.
As you build out your infection control plan and risk assessment goals, begin with taking time to assess your facility and staff. And if youre looking for a starting point as you create those goals, we recommend you start with an eye on these 5 attributes of high-performing infection prevention and control programs.
Read Also: Ear Infection That Will Not Go Away In Adults
Assessment Tool By Setting
Note: For Outpatient settings, the Guide to Infection Prevention for Outpatient Settings and its companion Checklist are consistent with the Outpatient Settings Infection Control Assessment Tool. While the same infection prevention elements are included in both the checklist and assessment tool, the facility demographics sections differ slightly. The assessment tool is intended for health department use whereas the checklist is intended primarily for healthcare facility use.
Realistic: Ask Your Staff For Suggestions
Realistic goals are rooted in people: Ask for input from the staff closest to the problems. Accrediting agencies often dont give specific instructions for this step, which means you have the freedom to include as much staff input as possible as you build your risk assessment. This assessment can take the form of surveys , committee participation and interviews. Include members of the infection prevention team, nurses, other clinicians, IT, and organizational leadership.
You May Like: Where To Go For A Sinus Infection
Helpful Resources To Support Nursing Homes With Infection Prevention During The Covid
Helpful resources to support nursing homes with infection prevention during the COVID-19 pandemic and beyond:
Infection Prevention Assessment Tools, Resources and Trainings:
- Post COVID-19 Outbreak Guide After a COVID-19 outbreak, what do you do? This guide tool provides step by step guidance to help your team recover and take action to improve prevention practices.
- Infection Prevention Resource List A one-stop shop for infection prevention resources provided and updated by Telligen.
- Guidebook for Infection Prevention and Control Preparedness A resource to assist nursing homes with infection prevention quality improvement initiatives. The guidebook includes information, strategies, and example process measures to guide you through a PDSA cycle based on your IP assessment improvement areas.
- IPC Risk Assessment A tool to help focus improvement activities on essential tasks to reduce infection control risks. Completing an infection control risk assessment can help improve resident and staff safety, identify training opportunities, and uncover prevention practice gaps while assessing the probability of infection transmission.
- Infection Prevention and Control Assessment Tool for Long Term Care Facilities A tool intended to assist in the assessment of infection control programs and practices.
Root Cause Analysis Tools:
Plan Do Study Act Tools:
Process and Audit Tools:
The Smart Approach To Infection Control Risk Assessment
Infection control teams are facing the biggest disruption the field has seen in years.
Thanks to the evolving COVID-19 pandemic, shifting care models and an aging population, infection prevention and control leaders will need to rethink and refresh the way they approach risk assessment going forward.The specifics of your IPC risk assessment a detailed review of potential risk factors for infection related to the care and services you provide will vary depending on your goals and risk profile. Focusing on SMART elements will help ensure a solid foundation as you customize your risk assessment and infection control plan.
Read Also: What Kind Of Antibiotics Are Good For Tooth Infection