Risk Factors For Group B Streptococcal Infection
If a pregnant woman is found to be a GBS carrier, the infection can easily be treated with intravenous antibiotics. Risk factors that may prompt your obstetrician to screen for GBS infection include:
- a GBS-positive swab in a previous pregnancy
- a previous baby with GBS infection
- pre-term labour
- rupturing of the membranes well before the onset of labour
- signs of infection around the time of labour or delivery
- prolonged labour.
For non-pregnant women and others, chronic diseases such as diabetes or cancer make you more vulnerable to getting GBS infection.
Group B Strepinfection In Adults
GBS can occasionally cause other infection in adults.
When GBS infection occurs in adults, its usually in those with serious underlying medical conditions which reduce the effectiveness of the immune system and so make them more susceptible to all kinds of infection, including GBS in the elderly and in pregnant women. Although uncommon, GBS infection in adults displays a whole spectrum of severity, from easily treated to very serious, particularly in non-pregnant adults.
GBS infections in adults are usually skin and soft tissue infections , blood infections, pneumonia and urinary tract infections . GBS may also cause meningitis in adults, as well as bone infections and deep eye infections.
The overall rate of GBS bacteraemia for 2018 was 4.2 per 100,000 population for England, Wales and Northern Ireland combined, with 11% more cases reported compared to 2015. Rates were highest in those aged less than one year . In adults, rates of GBS bacteraemia were highest in those aged 75 and over .
Impact Of Study Quality Maternal Condition And Gestational Ages
In subgroup analysis by study quality , we found a similar efficacy in prevention of all cause infections , GBS infection , EOGBS infection , non-GBS infections , and GBS colonization between two groups. The number of studies on other outcomes was too small to perform subgroup analysis on. In subgroup analysis by maternal conditions , we found a similar efficacy in prevention of all cause mortality , mortality from EOGBS infection , all cause infections , GBS infection , EOGBS infection , non-GBS infections , and GBS colonization between two groups. In subgroup analysis by gestational ages , we found a similar efficacy in prevention of all cause infections , GBS infection , EOGBS infection , non-GBS infections , and GBS colonization between two groups.
Table 3. Effect comparison of subgroups of study quality.
Table 4. Effect comparison of subgroups of maternal conditions.
Table 5. Effect comparison of subgroups of gestational ages.
You May Like: Urgent Care Or Er For Kidney Infection
How Do People Get Group B Strep
In newborns, group B Streptococcus infection is acquired through direct contact with the bacteria while in the uterus or during birth thus, the gestational bacterial infection is transmitted from the colonized mother to her newborn. Approximately 50% of colonized mothers will pass the bacteria to their babies during pregnancy and vaginal birth. However, not all babies will be affected by the bacteria, and statistics show that about only one of every 200 babies born to a GBS-colonized mother will go on to develop a GBS infection.
Group B strep infection is more common in African Americans than in whites. There are also maternal risk factors that increase the chance of transmitting group B Streptococcus to the newborn leading to early-onset disease:
- Labor or membrane rupture before 37 weeks gestation
- Membrane rupture more than 18 hours before delivery
Oral Antibiotics In Labor
I know that oral antibiotics are not acceptable protocol and the reasoning is that the antibiotics don’t get across the placenta in a timely fashion. Does anyone use them anyway, and is there any place I can look to find out how long it does take to get the antibiotics to get into the placenta? My understanding, a while back, is that it is not used, and hasn’t really been studied, but I don’t know if that is still true.
I do, start about a week before and hope she goes into labor in the time frame but can continue another round.
I am a homebirth midwife and here is my method for detecting and dealing with strep.
I culture at 36 weeks, if the mom is positive I give Amoxicillin 500 mg q 6h for 10 days. If she goes overdue I will reculture at 41 weeks. Depending on the situation I may or may not culture Mom at the beginning of labor but it is an option while closely observing baby for the next few days.
The good news is, IV antibiotics are NOT required. My CNM is putting me on oral antibiotics. I will take 3 a day starting at week 37 and then one a day until labor begins. When labor begins, I will take one every 4-6 hours until the baby is born. It seems like a lot, but it is better than being stuck in the hospital!
Treatment for GBS at a Homebirth in an Illegal State
One option would be to follow the common protocol of treating only for risk factors, even for women who are GBS positive.
Or you could take a little vacation south of the border. 🙂
Don’t Miss: Can You Give Yourself A Yeast Infection
What Tests Do Health Care Professionals Use To Diagnose Group B Strep Infection
In newborns and adults, isolation of the GBS bacteria is necessary for a definitive diagnosis. Laboratory studies that isolate the organism from certain body fluids, such as blood, cerebrospinal fluid , and urine, help establish the diagnosis. For screening of pregnant women, a health care professional will obtain a swab of a woman’s vaginal and rectal area to screen for GBS infection at 35-37 weeks of gestation. Test results can take a few days. A lumbar puncture may need to be performed when meningitis is suspected. A health care professional may order imaging studies such as a chest X-ray to evaluate whether pneumonia is present.
Treatment Of Streptococcal Skin Infection
It can be difficult to distinguish clinically between skin infection caused by streptococci and other bacteria such as Staphylococcus aureus. Antibiotics should therefore be chosen to cover the most likely organisms. Flucloxacillin is more appropriate than simple penicillin as it treats both Staphylococcus and strep.
If the laboratory has confirmed streptococcal infection, then the most appropriate antibiotic is usually penicillin. All streptococci in the Lancefield group are very sensitive to penicillin. Those patients with penicillin allergy may be given erythromycin or a cephalosporin , which are effective against most streptococci although some erythromycin resistance is emerging. In very severe S. pyogenes infections, such as necrotising fasciitis, clindamycin may be added to penicillin as very large numbers of bacteria may overwhelm penicillin’s mechanism of action.
Pneumococcal skin infections are generally treated with penicillin but low levels of resistance have recently been reported. In more serious infections, ceftriaxone or vancomycin may be more appropriate.
Recommended Reading: Pain Meds For Urinary Tract Infection
If You Are Having A Planned Caesarean Section
If you are carrying GBS and have a caesarean section planned , you do not need antibiotics to prevent GBS infection in your baby. This is unless labour has started or your waters have broken.
All women having a caesarean section will be offered antibiotics at the operation. This is to reduce the risk of a wide variety of infections, including GBS.
I had tested positive for GBS during previous pregnancies, so I was offered antibiotics during labour with my youngest son. I was being induced due to an unrelated complication and had a history of fast deliveries and so was given my first dose of antibiotics before having my waters manually broken. It ended up being my only dose as our little boy was born 3 hours later. Having the drip didn’t affect my labour at all, I was mobile and active during labour. It gave us enormous peace of mind to know that the antibiotics had minimised the chance of him developing a GBS related infection.
Fiona
What Could Gbs Mean For My Baby
Many babies come into contact with GBS during labour or around birth and most of them will stay healthy.
However, some of these babies become seriously ill. Around 1 in every 1,750 newborn babies in the UK and Ireland become unwell in the first week after birth, usually within 12-24 hours of birth. This is known as early-onset GBS infection.
GBS can cause infections such as sepsis, pneumonia and meningitis. A small number of babies who recover from GBS infection will have a long-term disability. Sadly, a small number of babies who develop an early-onset GBS infection die.
However, although GBS infection can make your baby very unwell, most babies will make a full recovery with early treatment.
“I wasn’t tested for GBS but it was discovered following a urine sample when I was around 16 weeks pregnant. It was really stressful being diagnosed with group B strep – my pregnancy was tense anyway because I’d already had a son who was stillborn. I was given antibiotics during labour and thankfully our daughter was born safe and well and is now a very boisterous 6 year-old.”
Jennifer
Recommended Reading: Urinary Tract Infection Blood In Pee
How Does Group B Strep Affect Babies
When women with GBS are treated with antibiotics during labor, most of their babies do not have any problems. But some babies can become very sick from GBS. Premature babies are more likely to be infected with GBS than full-term babies because their bodies and immune systems are less developed.
The two types of GBS disease in babies are:
Pearls And Other Issues
- In the United States of America, GBS is known to be the most common infectious cause of morbidity and mortality in neonates.
- Intrapartum antibiotic prophylaxis is only effective in the prevention of early-onset GBS infection.
- The CDC recommends universal screening with GBS rectovaginal culture between 35 to 37 weeks in each pregnancy.
- Intrapartum antibiotic prophylaxis is recommended with positive GBS rectovaginal culture, GBS bacteriuria at any time during the pregnancy, or a history of delivery of infant affected by early onset GBS infection.
- If GBS status is unknown, antibiotic prophylaxis is recommended during preterm labor and delivery , in the presence of maternal fever during labor, or with prolonged rupture of membranes .
- Intravenous Penicillin G is the antibiotic of choice for intrapartum prophylaxis.
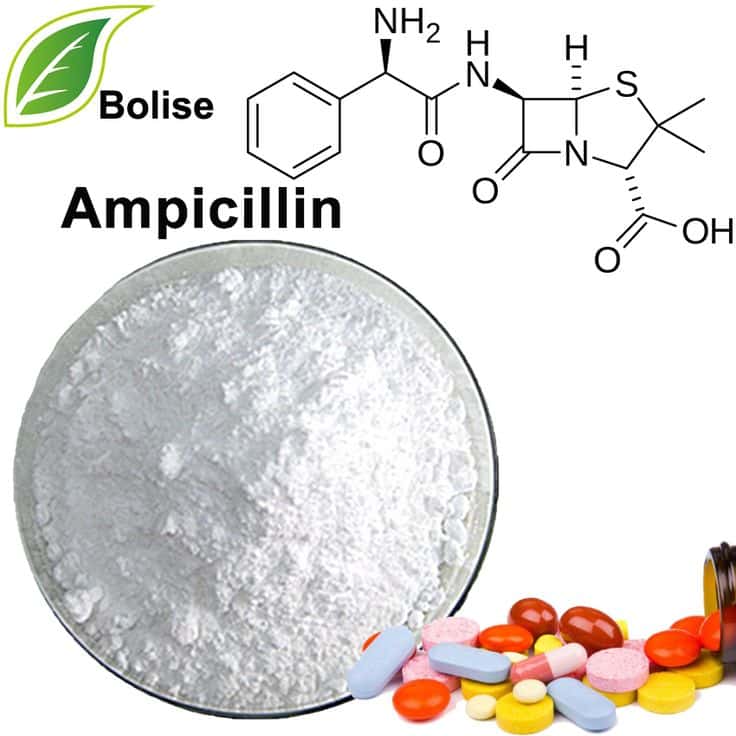
- Additional options for antibiotic prophylaxis are ampicillin, cefazolin, clindamycin, or vancomycin.
You May Like: How To Get Rid Of A Bacterial Infection Without Antibiotics
Antibiotic Prevention For Maternal Group B Streptococcal Colonization On Neonatal Gbs
- School of Public Health, Guangdong Pharmaceutical University, Guangzhou, China
Maternal colonization with group B Streptococcus during pregnancy increases the risk of neonatal infection by vertical transmission. However, it remains unclear whether treating all colonized women during labor exposes a large number of their neonates to possible adverse effects without benefit. We performed a meta-analysis to assess the effect of intrapartum antibiotic prophylaxis on neonatal adverse outcomes. We identified studies by searching several English and Chinese electronic databases and reviewing relevant articles. Data were pooled using fixed-effects or random-effects meta-analysis, and for each outcome both risk ratio and 95% confidence intervals were calculated. Fourteen studies were included, comprising 13 randomized clinical trials and 1 cohort study. Antibiotic prophylaxis is associated with a significant reduced risk of all cause infections , GBS infection , early-onset GBS infection , non-GBS infections , and GBS colonization . But no significant reduction was observed in late-onset GBS infection, mortality from early-onset GBS infection or from non-GBS infections. Notably, no significant differences were found between ampicillin and penicillin prevention for neonatal adverse outcomes. Our findings suggest that antibiotic prophylaxis is effective in reducing neonatal GBS colonization and infection.
Will Ibe Tested For Group B Strep
Yes, your healthcare provider will test you for GBS late in your pregnancy, around weeks 36 to 37.
Your obstetrician uses a cotton swab to obtain samples of cells from your and rectum. This test doesn’t hurt and takes less than a minute. Then, the sample is sent to a lab where it’s analyzed for group B strep. Most people receive their results within 48 hours. A positive culture result means you’re a GBS carrier, but it doesn’t mean that you or your baby will become sick.
If youre using a midwife, you might be given instructions on how to test yourself at home and submit the swab to a lab.
Also Check: Common Treatment For Sinus Infection
Symptoms Of Gbs Infection
Many people with GBS may not know that these bacteria are living in their body, and they might never experience any symptoms. They may only find out if they undergo a test in the doctors office.
When the bacteria cause an infection, the symptoms can vary among individuals and will depend on the part of the body where the infection occurs.
In adults, common symptoms include fever, chills, and general fatigue. GBS may also cause other serious infections, including infections in the urinary tract, throat, or blood.
Serious symptoms include issues such as:
- rapid breathing
- low alertness or brain fog
- swelling near an infected area
- inability to use a muscle or joint
Anyone experiencing serious symptoms such as these should seek immediate medical attention.
Most pregnant women who carry group B strep will not show any signs or symptoms, even if they can pass it on to their child during labor.
However, GBS may cause pregnancy-related issues, including stillbirth, miscarriage, and preterm delivery.
As many other factors can also lead to these issues, most of the time, doctors will not know the direct cause.
In newborns, the symptoms of GBS infection are much more likely to become serious, although they can initially resemble those of other health issues.
Symptoms in newborns can include:
- difficulty breathing
- a blueish tint to the skin
Group B Streptococci/streptococcus Agalactiae
GBS infection is typically due to colonization, usually asymptomatic, of the genital and/or gastrointestinal tract. These bacteria infect the placenta either by ascending through the cervix into the amniotic cavity or via the urinary tract resulting in urinary tract infection and bacteremia.24 GBS infection is particularly lethal to the fetus because it can cause pneumonia and sepsis. For this reason, it was the focus of a recent late pregnancy screening and treatment protocol in the United States.39-41 Infection during pregnancy can occur in the absence of ruptured membranes.13 Classically, GBS causes a necrotizing chorioamnionitis of high maternal and fetal stage .42,43 Rapid bacterial growth often allows the organisms to be readily visualized on the placental membranes . In cases of retained stillbirth, especially in the second trimester, one can occasionally see organisms filling the villous vascular spaces . The usual histology of ACA due to GBS amnionic fluid infection is nonspecific, but if necrotizing ACA is present, GBS should be strongly suspected, especially if there is high fetal and maternal stage. Umbilical cord involvement is usually limited to the vessels, but, in some cases, small surface abscesses may be present , different from the larger abscesses seen with candidal omphalitis .
Drucilla J. Roberts, in, 2010
You May Like: Male Urinary Tract Infection Treatments
What Are The Signs And Symptoms Of A Gbs Infection In Babies
GBS infection in babies may be grouped into early-onset and late-onset GBS infection. Early-onset GBS infection occurs within the first week of life, usually within 72 hours of birth. Late-onset GBS infection commonly appears after the first week of birth. Your baby may have any of the following:
- Eating poorly or vomiting
- Fast or slow heartbeat and trouble breathing
- Fever, hypothermia , or seizures
- Irritability, drowsiness, or difficulty waking up
- Sensitivity to bright lights
What To Do If You’re Worried About Gbs
Understandably, some women feel anxious about not having a routine test for GBS. Its best to talk to your midwife or GP if you have any concerns about GBS. Although testing isnt routinely offered to all pregnant women, you can pay for a test privately.
You can find information about getting tested for GBS on the Group B Strep Support website.
You May Like: Does Monistat Get Rid Of Yeast Infection
Treating Gbs Infection In Adults
Early recognition and treatment is important to cure GBS infection in adults. High doses of antibiotics such as penicillin should be administered and the full course taken.
Most GBS infection can be treated successfully, although some people will require all the expertise of intensive care facilities. Not all hospitals have such a facility and so some ill patients will have to be transferred to one with these specialised facilities.
GBS infections, especially the more deep-seated ones, require expert care, prolonged courses of antibiotics and sometimes more than one antibiotic at the same time. In some cases, surgery may be necessary to drain infected sites and remove damaged tissue. Due to the varied nature of these infections, it is impossible to generalise about what is the most appropriate treatment.
If you have any questions about Group B Strep, please call our helpline
Mon-Fri 9am-5pm
What Can Complicate A Group B Streptococcal Infection
Pregnant women who have become unwell from a GBS infection are more likely to go into labour before their babys due date, and although rare, their baby is more likely to be stillborn. If you are pregnant and found to have a GBS infection, you will be treated with antibiotics to protect you and your baby.
Babies are more likely to become infected with GBS if they are born before 37 weeks of pregnancy, if their mother has a high temperature during labour or on the day after, or had a prior pregnancy or baby infected with GBS.
In cases of a severe infection, GBS can cause a blood infection or an infection of the membranes surrounding the brain and spinal fluid .
Read Also: Does Cephalexin Treat Bacterial Infections