Right Data & Right Tools
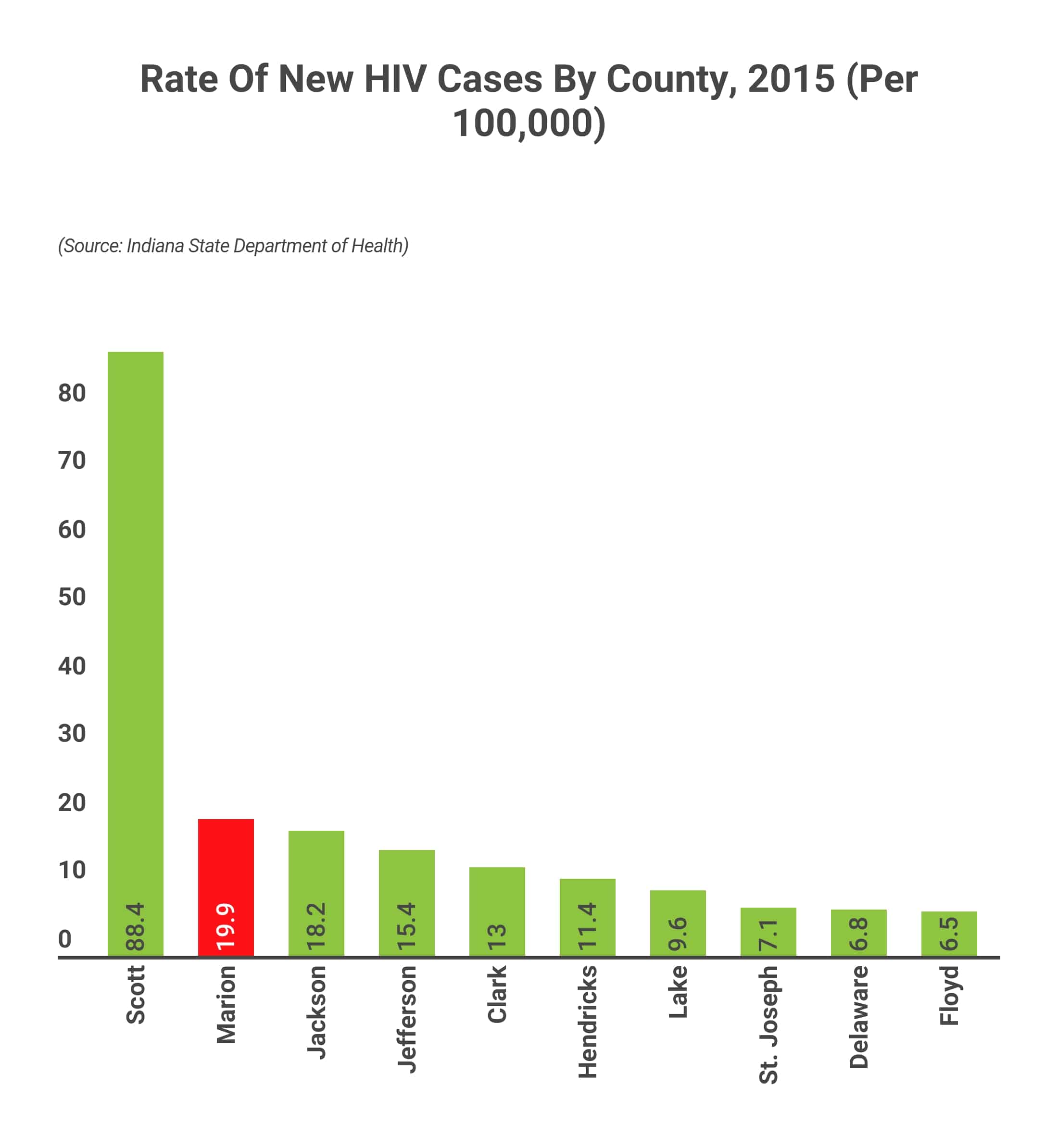
Data tell us that most new HIV infections occur in a limited number of counties and among specific populations, giving us the information needed to target our efforts to those locales that will make the biggest impact on ending the HIV epidemic. Further, today we have the tools available to end the HIV epidemic. Landmark biomedical and scientific research advances have led to the development of many successful HIV treatment regimens, prevention strategies, and improved care for persons living with HIV. Notably:
With these powerful data and tools, we have a once-in-a-generation opportunity to end the HIV epidemic.
Impact On Gay And Bisexual Men
- While estimates show that gay and bisexual men comprise only about 2% of the U.S. population, male-to-male sexual contact accounts for most new HIV infections and most people living with HIV .58
- Annual new infections among gay and bisexual men declined overall between 2015 and 2019 but remained stable among Black and Latino gay and bisexual men.59
- Blacks gay and bisexual men accounted for the largest number of new diagnoses among this group in 2019, followed by Latino gay and bisexual men .60 Additionally, according to a recent study, Black gay and bisexual men were found to be at a much higher risk of being diagnosed with HIV during their lifetimes compared with Latino and white gay and bisexual men.61 Young Black gay and bisexual men are at particular risk â Black gay and bisexual men ages 20-29 accounted for 51% of new diagnoses among that age group and 13% of all diagnoses.62
Hiv By The Numbers: Facts Statistics And You
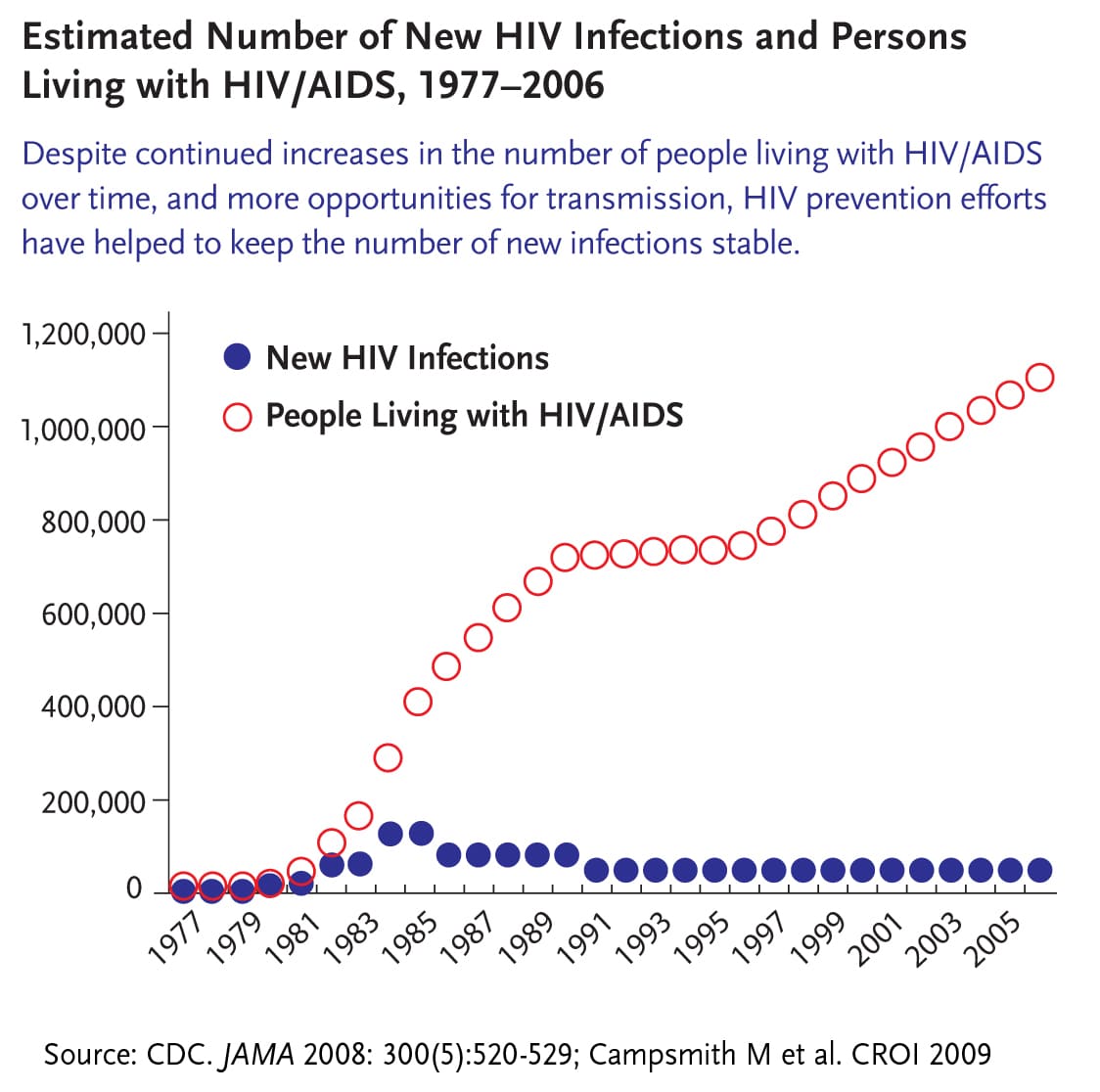
Centers for Disease Control reported the first five known cases of complications from HIV in Los Angeles in June 1981. The previously healthy men had contracted pneumonia, and two died. Today, more than a million Americans have the virus.
Being diagnosed with HIV was once a death sentence. Now, a 20-year-old with HIV who begins treatment early can expect to live to their
of people ages 13 and older with HIV dont know they have it.
An estimated 39,782 Americans were newly diagnosed with HIV in 2016. In that same year, 18,160 individuals living with HIV developed stage 3 HIV, or AIDS. This is in striking contrast to the early days of HIV.
According to the American Federation of AIDS Research, by the end of 1992, 250,000 Americans had developed AIDS, and 200,000 of these had died. By 2004, the number of cases of AIDS reported in the United States closed in on 1 million, with deaths totaling more than 500,000.
diagnosed in the United States in 2016, 2,049 men and 7,529 women contracted the virus. Overall, new diagnoses decreased.
When it comes to , 17,528 of those diagnosed in the United States in 2016 were black, 10,345 were white, and 9,766 were Latino.
Americans in the
AIDS.gov reports that 36.7 million people worldwide are living with HIV, and 35 million have died since 1981. Additionally, the majority of people with HIV live in developing and moderate-income nations, such as those in sub-Saharan Africa.
You May Like: Best Thing To Do For Tooth Infection
Why Is Monitoring Progress Important
Canada has endorsed the Joint United Nations Programme on HIV/AIDS and the World Health Organization global health sector strategy on HIV that includes global targets to generate momentum towards the elimination of AIDS as a public health threat by 2030.Footnote 1 The 90-90-90 targets state that by 2020, 90% of all people living with HIV know their status, 90% of those diagnosed receive antiretroviral treatment, and 90% of those on treatment achieve viral suppression. When these three targets have been achieved, at least 73% of all people living with HIV will be virally suppressed. UNAIDS modelling suggests that achieving these targets by 2020 will enable the world to eliminate the AIDS epidemic by 2030.Footnote 1
The continuum of HIV care is a useful framework for assessing progress against the 90-90-90 targets. The sequential nature of the stages in the continuum can point to where efforts need to be focussed and which areas require improvement. Estimating HIV prevalence is the first step in the continuum of care, and is critical for guiding the planning and investment for treatment, care and ongoing support for people living with and affected by HIV and AIDS. In addition, understanding HIV incidence is fundamental for understanding temporal changes in transmission patterns, and is useful for public health decision makers to monitor, strengthen and evaluate the impact of multi-sectoral public health actions.
Recommended Reading: Emergency Antibiotics For Tooth Infection
A Major Health Crisis
Since the early 1980s, when the first cases were diagnosed in the USA, an estimated 78 million people have been infected by HIV and 39 million people have died of AIDS and AIDS-related illnesses. There are currently 36.9 million cases worldwide, according to UNAIDS.
Every year the number of people living with HIV increases, a fact that can be interpreted both positively more people have access to antiretroviral treatment and negatively the HIV/AIDS pandemic continues.
Breakthroughs but no stop to the rise in new infections
The availability of triple antiretroviral therapy in the mid-1990s marked the transition from fatal disease to chronic infection. But despite the enormous progress achieved with HIV, global efforts to prevent and control new infections continue to encounter obstacles.
Worrying numbers of people contract the virus each year: 2 million people were infected in 2014 and 1.2 million people die from HIV every year.
A global health problem
Some 80% of people living with the virus areconcentrated in just 20 countries: South Africa, Nigeria, India, Zimbabwe, Mozambique, Tanzania, Uganda, Kenya, the USA, Russia, Zambia, Malawi, China, Brazil, Ethiopia, Indonesia, Cameroon, Ivory Coast, Thailand and the Democratic Republic of Congo.
However, HIV/AIDS continues to be a global health problem. The rate of new infections and deaths has seen an increase in recent years in some regions of Asia, the Pacific, the Middle East and North Africa.
Also Check: Does Nuvaring Cause Yeast Infections
Impact Across The Country
- Although HIV has been reported in all 50 states, the District of Columbia, and U.S. dependencies, the impact of the epidemic is not uniformly distributed.
- Ten states accounted for about two-thirds of HIV diagnoses among adults and adolescents in 2019 .31 Regionally, the South accounted for more than half of HIV diagnoses in 2019.32
- Rates of HIV diagnoses per 100,000 provide a different measure of the epidemicâs impact, since they reflect the concentration of diagnoses after accounting for differences in population size across states. The District of Columbia has the highest rate in the nation, compared to states, nearly 3 times the national rate and Georgia was the state with highest rate , twice that of the national rate.33,34 Nine of the top 10 states by rate are in the South.35
- New HIV diagnoses are concentrated primarily in large U.S. metropolitan areas , with Miami, Orlando, and Atlanta topping the list of the areas most heavily burdened.36
| Table 1: Top Ten States/Areas by Number and Rate of New HIV Diagnoses , 2019 | |
| State | |
| U.S. Rate | 13.2 |
| CDC. HIV Surveillance Report, Diagnoses of HIV Infection in the United States and Dependent Areas, 2019 vol. 32. May 2021. |
Social Determinants Of Health 2019
Percent of Population with a High School Education, 2019 88.6%
Income Inequality , 2019 0.481
Percent of Population Living in Poverty, 2019 12.3%
Median Household Income, 2019 $65,712
Percent of Population Lacking Health Insurance, 2019 10.4%
Percent of Population Unemployed, 2019 3.7%
Percent of Population Living with Food Insecurity, 2016-2019 10.5%
Percent of Population Living in Unstable Housing, 2019 13.7%
Read Also: Do I Have A Kidney Infection Or Uti
What Are The Implications For Public Health Practice
HIV treatment and prevention services should be tailored to the most affected communities and their service providers and address social and economic obstacles contributing to HIV-related health disparities. Ending the HIV epidemic requires equitable implementation of prevention tools to diagnose HIV infection early, treat persons with HIV to rapidly achieve viral suppression, and link persons to preventive services.
The Global Distribution Of Deaths From Hiv/aids
In some countries HIV/AIDS is the cause of more than a quarter of all deaths
Globally, 1.5% of deaths were caused by HIV/AIDS in 2019.
This share is high, but masks the wide variations in the toll of HIV/AIDS across the world. In some countries, this share was much higher.In the interactive map we see the share of deaths which resulted from HIV/AIDS across the world. Across most regions the share was low: across Europe, for example, it accounted for less than 0.1% of deaths.
But across some countries focused primarily in Southern Sub-Saharan Africa the share is very high. More than 1-in-4 of deaths in South Africa were caused by HIV/AIDS in 2019. The share was also very high across Botswana Mozambique Namibia Zambia Kenya and Congo .
Death rates are high across Sub-Saharan Africa
The large health burden of HIV/AIDS across Sub-Saharan Africa is also reflected in death rates. Death rates measure the number of deaths from HIV/AIDS per 100,000 individuals in a country or region.
In the interactive map we see the distribution of death rates across the world. Most countries have a rate of less than 10 deaths per 100,000 often much lower, below 5 per 100,000. Across Europe the death rate is less than one per 100,000.
Across Sub-Saharan Africa the rates are much higher. Most countries in the South of the region had rates greater than 100 per 100,000. In South Africa and Mozambique, it was over 200 per 100,000.
Recommended Reading: Farxiga Side Effects Yeast Infection
People Living With Hiv
San Francisco has one of the largest populations of people living with HIV in the United States with an estimated 15,811 people living with HIV .
Of the total number of San Franciscans living with HIV/AIDS at the end of 2020, 8,950 were living with HIV ever classified as AIDS. AIDS is a late-stage HIV disease defined by a low count of CD4 cells or an opportunistic infection .
As of December 2020, 71% of people living with HIV in San Francisco were over age 50 .
Annual New Hiv Infections In The Us Down 73% Since 1980s Cdc Estimates
The number of new yearly HIV infections in the U.S. has decreased by 73% since the peak of the HIV/AIDS epidemic during the mid-1980s, the Centers for Disease Control and Prevention estimated in a new report.
“Despite the lack of a cure or a vaccine, today’s HIV prevention tools, including HIV testing, prompt and sustained treatment, preexposure prophylaxis, and comprehensive syringe service programs, provide an opportunity to substantially decrease new HIV infections,” the CDC stated. It recommended “intensifying efforts to implement these strategies equitably” to continue reducing transmission, illnesses and deaths.
The estimates were calculated by analyzing data from the National HIV Surveillance System. The CDC study estimated 2.2 million total new HIV infections between 1981 to 2019. Using those numbers, researchers compared trends by sex at birth, race and ethnicity, and transmission category.
Their analysis showed that male-to-male sexual contact accounted for more than half of infections each year, except for 1988 to 2002 when heterosexual sex was a greater factor. Those who inject drugs saw the largest relative reduction in HIV incidence during the past four decades. And females made up a larger proportion of infections in 2019 than during the epidemic’s peak.
Another recent report from the CDC found that about 4 in 10 transgender women surveyed in seven major U.S. cities have HIV.
Read Also: Keflex Used For Tooth Infection
How Does Cdc Know The Number Of People Living With Hiv If Some Of Those People Are Unaware Of Their Status
CDC estimates the number of people living with HIV by using a scientific model. This model helps CDC estimate the number of new HIV infections and how many people are infected but dont know it. HIV prevalence is the number of people living with HIV infection at a given time, such as at the end of a given year. More information on HIV prevalence.
Cdc To Target Proven Prevention Efforts
That’s why universal HIV testing is the cornerstone of the CDC’s HIV prevention program. But Frieden was quick to note that testing is only part of the solution.
“What we have come to understand is the linkage between treatment and prevention,” he said. “But it is not enough to promote testing and linkage to care. We have to promote treatment and continuity of care. We have to make sure people with HIV live long, healthy lives and that we reduce the risk of those around them as well.”
Don’t Miss: Male Urinary Tract Infection Treatments
The Cultural Response To Hiv
Public response was negative in the early years of the epidemic.
In 1983, Dr. Joseph Sonnabend in New York was threatened with eviction for treating people with HIV, leading to the first AIDS discrimination lawsuit.
Bathhouses across the country closed due to sexual activity and the associated risk. Some schools also barred children with HIV from attending.
U.S. blood banks started screening for HIV in 1985, and men who had sex with men were banned from donating blood . first lifted some of its restrictions in December 2015. The FDA loosened its restrictions again in 2020, motivated by the blood shortage caused by COVID-19.)
In 1987, the United States placed a travel ban on visitors and immigrants with HIV.
The United States government resisted funding needle exchange programs due to the War on Drugs. NEPs were shown to be effective at reducing HIV transmission.
In 1997, researchers calculated that this resistance accounted for .
The number of avoidable transmissions may be even higher.
A 2005 study looked at people in New York City who used injectable drugs and had been admitted to a drug detoxification program. The researchers concluded that the legalization of syringe exchange programs helped reduce HIV prevalence among this group from 50 percent in 1990 to 17 percent in 2002.
Association Between Recent Infections And Other Variables
The univariate logistic regression revealed that several factors were associated with recent HIV infection, such as mode of transmission, age, gender and region of infection, which are shown in Table Table2.2. These associations were confirmed by multivariable logistic regression, which showed that cases with a different mode of transmission than MSM were more likely to have a long-standing HIV infection. Including persons younger than 25 years, the proportion of persons with long-standing HIV infections increased with age .
An additional multivariable logistic regression aimed to identify sub-groups within the main transmission groups revealed, that female German intravenous drug users had a higher chance of being diagnosed with a recent HIV infection than German MSM .4). However, the numbers of female German drug users were small, with 28 cases of recent HIV infection among 49 female German drug users in total. Other groups with a lower chance of being recently infected with HIV compared to German MSM were German heterosexual females , heterosexual females with an origin abroad , heterosexual females with an unknown origin and heterosexual men with an origin abroad .
Don’t Miss: How To Treat A Bacterial Throat Infection
Impact On Young People
- Teens and young adults continue to be at risk, with those under 35 accounting for 57% of new HIV diagnoses in 2019 .51 Most young people are infected sexually.52
- Among young people, gay and bisexual men and minorities have been particularly affected.53
- Perinatal HIV transmission, from an HIV-infected mother to her baby, has declined significantly in the U.S., largely due to increased testing efforts among pregnant women and ART which can prevent mother-to-child transmission.54,55,56
- A recent survey of young adults found that HIV remains a concern for young people, especially for young people of color.57
New Hiv Infections Rose More Than 20% In Latin America In The Last Decade Paho Says
In another grave trend, COVID-19 disruption to health services threatens testing and treatment. PAHO and UNAIDS Launch Campaign to Promote HIV Self-Testing
Washington DC, November 30, 2020 – New yearly infections from the HIV virus rose 21% from 2010 through 2019 in Latin America, the Pan American Health Organization said today. Meanwhile, deaths from AIDS-related illnesses declined by only a slight 8% in the last decade in Latin America. In comparison, AIDS-related deaths dropped by 37% in the Caribbean.
The number of annual new infections has continued to rise, reaching 120,000 in 2019 compared to 100,000 in 2010, PAHO said, based on recently available data. Over the same time period, the number of annual AIDS-related deaths has dropped slightly to 37,000 in 2019 from 41,000 in 2010.
These data signal that HIV unequivocally still represents a major public health problem in Latin America, and we must tackle inequities, stigma and discrimination to ensure no one is left behind, PAHO Director Carissa F. Etienne said. And COVID-19 is expected to exacerbate this situation due to its impact on essential health services, especially in countries with fragile health systems. For these reasons, we must redouble our efforts to protect services and maintain our focus on the ultimate goal of eliminating AIDS, which cause untold human suffering.
Continuing stigma around HIV and AIDS, as well as unequal access to health services, also deter progress toward eliminating the disease.
You May Like: Can A Tooth Infection Heal On Its Own