Signal Transduction Through Ccr5 And Cxcr4
CCR5 and CXCR4 are both members of the seven-transmembrane-spanning family of heterotrimeric GPCRs. This family of proteins is characterized by an extracellular amino-terminal domain, seven membrane-spanning domains that form three extracellular and three intracellular loops, and a cytoplasmic tail domain. The amino terminus and three ECLs together form the binding pocket for the cognate chemokines, which appear to attach to their receptor and transmit signals in a two-site binding process . The intracellular loops and cytoplasmic tail bind to the heterotrimeric G proteins that in turn mediate effector functions.
A second series of experiments from Harmon and colleagues showed that HIV also signals through the Gq subunit, resulting in phospholipase C and Rac activation. Rac and the tyrosine kinase Abl then become linked to the Wave2 complex through the adapter proteins Tiam-1 and IRSp53, promoting Arp2/3-dependent actin nucleation and polymerization. Blocking activation of the Wave2 complex with small interfering RNAs or Abl kinase inhibitors arrested HIV entry at the hemifusion stage. Together, these experiments suggest a critical role for envelope-coreceptor signaling-induced actin remodeling during HIV entry, particularly in the case of resting CD4+ T cells.
Quantification And Statistical Analysis
Statistical details of experiments can be found in each figure legend. Nonparametric tests were used to compare medians between groups unless noted otherwise. The MannWhitney test was used for 2 groups and the KruskalWallis test followed by Dunns multiple comparison post-test was used for> 2 groups. Wilcoxon signed rank was used to compare continuous data between two time points. Spearmans correlation coefficients were used to examine associations between variables. Differences were considered significant at p< 0.05. For figures marked fold increase, the value at the final timepoint was compared to the initial timepoint rare values below 1 were normalized to the value of 1. Prism 8 was used for all analyses.
Hiv Infection Of Cd4+t Cells And Macrophages
For cell-free infection experiments, 2×104 infectious units of HIV, or for mock infection, media, were added to 105 cells in 100 l total volume for 12 h at 37 °C, then washed three times with PBS and replaced with 200 l media. Supernatant was collected for p24 measurement at days 1 , 2, 7, and 14. CD4+T cell cultures had low viability at day 14, consistent with prior literature, so samples were not collected at this point, and day 7 was the final timepoint. HIV p24 levels were measured by p24 ELISA .
You May Like: Does Yeast Infection Affect Pregnancy
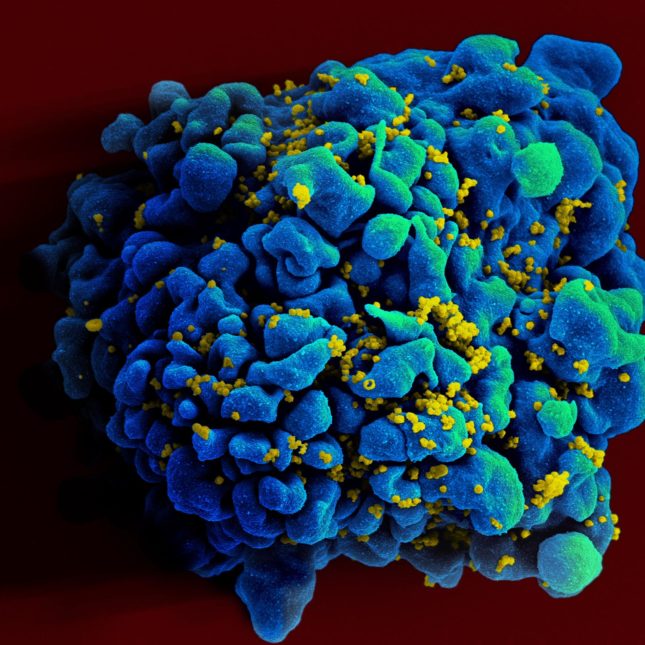
Contributors To Cd4+ T
CD4+ T-cells are known to be the central facilitators for both cellular and humoral immune responses against exogenous antigens and are kept constant in the human body by homeostatic mechanisms .HIV binds to the CD4 molecule on the surface of helper T-cells and replicates within them. This results in destruction of CD4+ T-cells and leads to a steady decline in this population of T-cells. The definition of progressive and slow loss of CD4+ T-cells is not clear. In order to understand the correlation between CD4+ T-cell depletion and immunopathogenesis, and its relationship with disease progression, a number of dynamic models have been put forward. Two of the most acknowledged mechanisms are discussed in detail in this review. These include direct virus attack leading to cytolytic effect and chronic immune activation resulting in apoptosis.
Pathophysiology Of Cd4+ T
- Division of HIV/AIDS, Department of Clinical Research, National Institute for Research in Tuberculosis , Chennai, India
The hall mark of human immunodeficiency virus infection is a gradual loss of CD4+ T-cells and imbalance in CD4+ T-cell homeostasis, with progressive impairment of immunity that leads ultimately to death. HIV infection in humans is caused by two related yet distinct viruses: HIV-1 and HIV-2. HIV-2 is typically less virulent than HIV-1 and permits the host to mount a more effective and sustained T-cell immunity. Although both infections manifest the same clinical spectrum, the much lower rate of CD4+ T-cell decline and slower progression of disease in HIV-2 infected individuals have grabbed the attention of several researchers. Here, we review the most recent findings on the differential rate of decline of CD4+ T-cell in HIV-1 and HIV-2 infections and provide plausible reasons for the observed differences between the two groups.
Don’t Miss: What Antibiotic Is Good For Tooth Infection
Interval Of Mild Or No Symptoms
After the first symptoms disappear, most people, even without treatment, have no symptoms or only occasionally have a few mild symptoms. This interval of few or no symptoms may last from 2 to 15 years. The symptoms that most commonly occur during this interval include the following:
-
Swollen lymph nodes, felt as small, painless lumps in the neck, under the arms, or in the groin
-
White patches in the mouth due to candidiasis
Some people progressively lose weight and have a mild fever or diarrhea.
These symptoms may result from HIV infection or from opportunistic infections that develop because HIV has weakened the immune system.
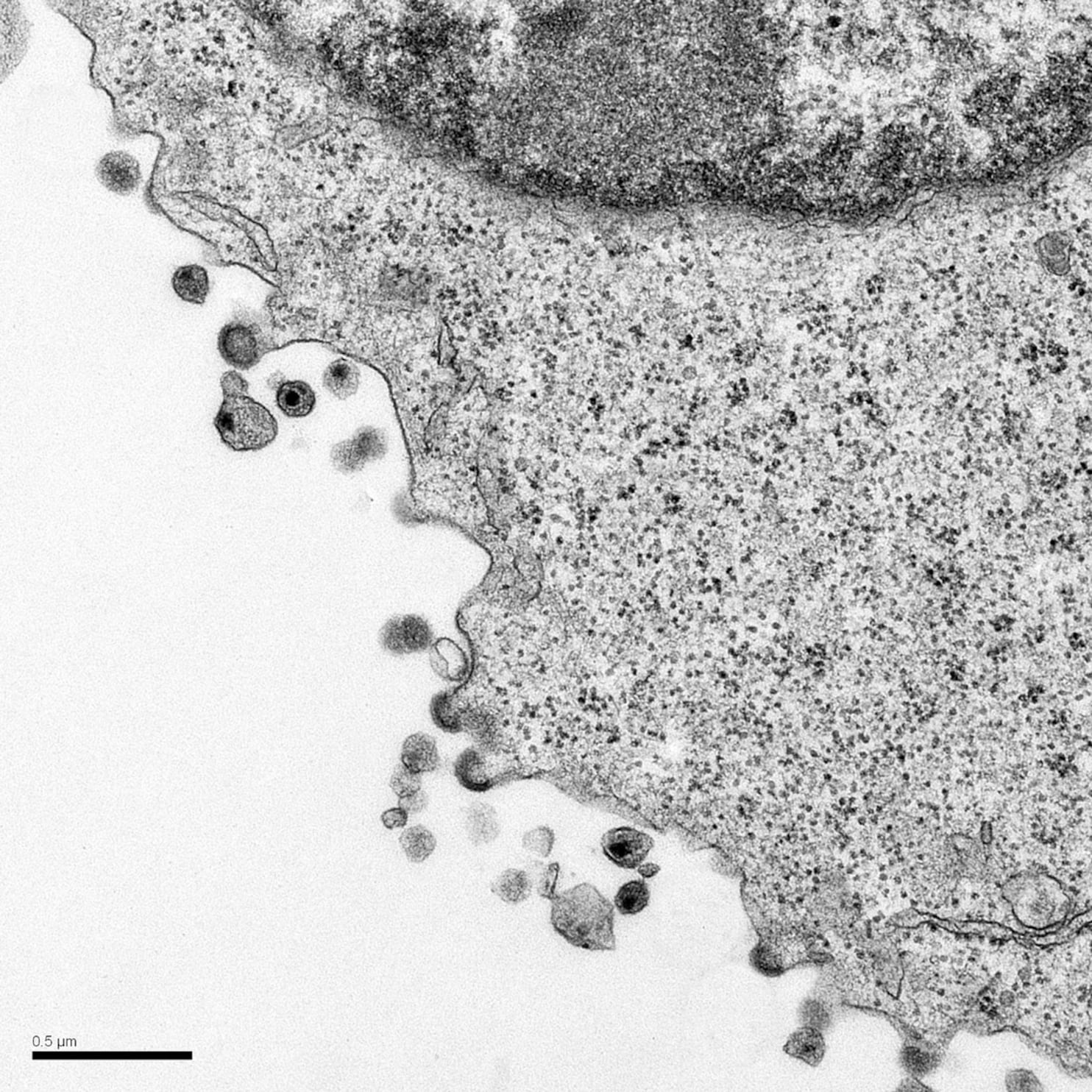
Cellcell Transfer And The Virological Synapse
In vitro, the rate-limiting step of virus infection is attachment to the host cell. In vivo, newly produced virions may well encounter an immediately adjoining, uninfected cell. In some cases, transfer of virus from one cell to another is a specialized process, as in the case of dendritic cells , which are professional antigen-presenting cells that scavenge the periphery, sampling antigen. They are commonly found in the mucosa and thus may be encountered by HIV during transmission. On antigen binding, DCs migrate to the lymph nodes, process, and present the antigen to T cells to trigger an adaptive immune response. DCs are relatively resistant to productive HIV infection owing to a combination of low CD4 and coreceptor expression, host restriction factors, postintegration HIV transcription blocks, and other unknown factors . However, they express a diverse range of attachment factors that facilitate the internalization and processing of pathogens before antigen presentation. HIV, along with viruses , can take advantage of this pathway to augment infection efficiency and dissemination .
Model of DC-mediated transinfection of CD4+ T cells. DCs capture and concentrate virions in trypsin-resistant surface-accessible compartments. CD4+ T cells, containing membrane protrusions, bind DCs. The CD4+ T-cell protrusions invade the virus-containing compartments and efficiently bind HIV. Virus then migrates toward the cell body to initiate infection.
Also Check: Will Nasacort Help Sinus Infection
How Do I Know If I Have Hiv
The only way to know for sure if you have HIV is to get tested. Testing is relatively simple. You can ask your health care provider for an HIV test. Many medical clinics, substance abuse programs, community health centers, and hospitals offer them too.
To find an HIV testing location near you, use the HIV Services Locator.
HIV self-testing is also an option. Self-testing allows people to take an HIV test and find out their result in their own home or other private location. You can buy a self-test kit at a pharmacy or online. Some health departments or community-based organizations also provide self-test kits for a reduced cost or for free.
Does Hiv Viral Load Affect Getting Or Transmitting Hiv
Yes. Viral load is the amount of HIV in the blood of someone who has HIV. If taken as prescribed, HIV medicine can reduce a persons HIV viral load very low level, which keeps the immune system working and prevents illness. This is called viral suppression, defined as having less than 200 copies of HIV per milliliter of blood.
HIV medicine can also make the viral load so low that a standard lab test cant detect it. This is called having an undetectable level viral load. Almost everyone who takes HIV medicine as prescribed can achieve an undetectable viral load, usually within 6 months after starting treatment.
As noted above, people with HIV who take HIV medicine as prescribed and get and keep an undetectable viral load can live long and healthy lives and will not transmit HIVto their HIV-negative partnersthrough sex.
HIV medicine is a powerful tool for preventing sexual transmission of HIV. But it works only if the HIV-positive partner gets and keeps an undetectable viral load. Not everyone taking HIV medicine has an undetectable viral load. To stay undetectable, people with HIV must take HIV medicine as prescribed and visit their health care provider regularly to get a viral load test. Learn more.
Recommended Reading: Male Urinary Tract Infection Treatments
How Does Hiv Destroy The Body
Activist Cleve Jones on finding out he was HIV positive
Almost immediately upon infection, the immune system recognizes that it is under attack. Many people experience flu-like symptoms, sometimes with a rash, two to three weeks after being infected. This is the body reacting to the invading HIV and mounting a terrific immune response, producing up to a billion helper and killer T-cells a day. At this point, there is enough virus in the blood that HIV can be diagnosed through a blood test.
Because the virus infects CD4 cells, stimulating the immune system means activating infected CD4 cells, which then produce more viruses. Those viruses in turn go out and infect more of the newly created CD4 cells.
AIDS activist Phill Wilson on watching his lover die from AIDS
Eventually HIV gains the upper hand and begins to kill off more CD4 cells than the body can produce. Without the CD4 cells, the B-cells and killer T-cells lack instruction about where to go and what to look for, and the body’s immune response becomes less and less effective.
Sudden Unexplained Weight Loss
National Human Genome Research Institute
Weight loss is common in people living with HIV during the advanced stages of the disease.
This type of weight loss is more than just a few poundsit’s a sudden, unexplained weight loss of 10% or more of a person’s body weight, in which both fat mass and lean muscle are lost.
The condition is also called HIV wasting syndrome. It’s not as common today as it once was because antiretroviral drugs keep the virus suppressed and allow the immune system to rebuild itself. Wasting is mainly seen in people who have not been treated for HIV.
The exact cause of HIV wasting is unknown, but it is thought that the constant inflammation caused by HIV makes the body burn energy faster and reduces testosterone levels .
Other causes of wasting include malnutrition, chronic diarrhea, tuberculosis, and cancerall of which require urgent diagnosis and treatment.
Don’t Miss: Severe Urinary Tract Infection Treatment
Hiv Latency Is Established Directly And Early In Both Resting And Activated Primary Cd4 T Cells
-
Affiliations Gladstone Institute of Virology and Immunology, San Francisco, California, United States of America, Biomedical Sciences Program, University of California, San Francisco, San Francisco, California, United States of America
-
Current Address: Molecular Cell and Developmental Biology Department, University of California, Los Angeles, Los Angeles, California, United States of America
Affiliation Gladstone Institute of Virology and Immunology, San Francisco, California, United States of America
-
* E-mail:
Affiliations Gladstone Institute of Virology and Immunology, San Francisco, California, United States of America, Department of Medicine, University of California, San Francisco, San Francisco, California, United States of America
How Does Hiv Spread Throughout The Body
HIV cannot reproduce on its own, so it must get into these cells so that it can copy itself.
First, the virus attaches itself to a T-helper cell and fuses with it . It then takes control of the cellâs DNA, makes copies of itself inside the cell, and finally releases more HIV into the blood.
HIV will continue to multiply and spread throughout the body. This is a process called theâ¯HIV lifecycle.
You May Like: Over The Counter Antibiotics For Throat Infection
Causes Of Hiv Infection
It’s a fragile virus and does not survive outside the body for long.
HIV cannot be transmitted through sweat, urine or saliva.
Other ways of getting HIV include:
- sharing needles, syringes or other injecting equipment
- transmission from mother to baby during pregnancy, birth or breastfeeding
The chance of getting HIV through oral sex is very low and will be dependent on many things, such as whether you receive or give oral sex and the oral hygiene of the person giving the oral sex.
Establishing A Reservoir For Hiv
Another potential contributor to the HIV reservoir is a less differentiated subset of long-lived memory T cells with a high self-renewal capacity known as stem-cell memory CD4+ T cells . TSCM can be differentiated from naïve T cells via TCR stimulation in vitro supporting the idea that naïve T cells represent the precursor to TSCM. TSCM retain many phenotypic characteristics of naïve T cells but additionally express memory T cell markers including CD95 and CD62L . TSCM are infected by HIV in vitro, however, only a small fraction of cells are able to support productive infection . Still, prolonged survival of TSCM indicate that they may become the dominating population in the reservoir after long term suppression when ongoing rounds of virus replication are halted and other memory T cell compartments decay. Indeed, Buzon et al. found TSCM infected cells contribute minimally after 1 year on suppressive therapy but their contribution increased after long term therapy . These findings suggest that HIV infected TSCM cells could comprise a viral niche that promotes long-term viral persistence. Furthermore, replication competent virus has been recovered from CD45+/CD62L+ memory T cells ex vivo . Given the potential for TSCM to survive for prolonged periods and maintain a high proliferative capacity, it is critical to determine the contribution of the TSCM compartment to the HIV reservoir.
Recommended Reading: Can A Doctor Help With Tooth Infection
What Questions Should I Ask My Doctor
- Am I at high risk for HIV?
- What can I do to reduce my risk of HIV?
- How can I make sure I take my medications correctly?
- What can I do to protect myself from other illnesses?
- How can prevent the spread of HIV?
- What do my test results mean?
- What do my blood counts mean?
- What vaccinations should I get?
A note from Cleveland Clinic
Treatments have come a long way since the height of the AIDS epidemic. You have the best chance of living a long life if youre diagnosed early and are able to get on and stick with ART medications. People living with HIV today are able to work, have active social lives and families, and pursue fulfilling relationships. In fact, this can have a positive impact on your well-being.
While weve come a long way with treatments, unfortunately, social stigmas around HIV still persist. In addition to the feelings of fear and uncertainty a new diagnosis can bring, you may wonder how those around you will respond. If youre hesitant to get tested or get treatment, or if you just arent sure what your next steps are, you can reach out to a community organization that specializes in HIV. Remember that you are deserving of support, compassion and high-quality healthcare.
Can Medications Prevent Hiv
There are medications that can help prevent HIV in people who have been exposed or are at high risk for exposure. These include pre-exposure prophylaxis and post-exposure prophylaxis .
Pre-exposure prophylaxis
PrEP is a pill you take every day if you dont have HIV but are at high risk of getting infected.
- You have a sexual partner with HIV.
- You havent consistently used a condom.
- In the past six months, youve been diagnosed with a sexually transmitted disease .
PrEP is also recommended if you dont have HIV, you inject drugs and at least one of the following is true:
- You inject drugs with a partner who has HIV.
- You share needles or other equipment to inject drugs.
PrEP is not a replacement for other preventative measures. You should still use condoms and avoid sharing needles to inject drugs while taking PrEP.
Post-exposure prophylaxis
PEP uses HIV medicines to try to prevent an HIV infection soon after you are exposed. PEP is for those who dont have HIV or dont know if they have HIV and think theyve been exposed through consensual sex, sexual assault, shared needles , or work.
You must start PEP within 72 hours of exposure and take it every day for 28 days. PEP is only for emergency use and does not replace other precautions, like condom use.
You May Like: Signs Your Tooth Is Infected
Preventive Treatment After Exposure
People who have been exposed to HIV from a blood splash, needlestick, or sexual contact may reduce the chance of infection by taking antiretroviral drugs for 4 weeks. These drugs are more effective when they are started as soon as possible after the exposure. Taking two or more drugs is currently recommended.
Doctors and the person who was exposed typically decide together whether to use these preventive drugs. They base the decision on the estimated risk of infection and the possible side effects of the drugs. If they do not know whether the source is infected with HIV, they consider how likely the source is to be infected. However, even when the source of the exposure is known to be infected with HIV, the risk of infection after exposure varies, depending on the type of exposure. For example, risk from a blood splash is less than that from a needlestick.
Immediately after exposure to HIV infection, what is done depends on the type of exposure:
-
If skin is exposed, it is cleaned with soap and water.
-
Puncture wounds are cleaned with antiseptic.
-
If mucous membranes are exposed, they are flushed with large amounts of water.
Simplified Life Cycle Of The Human Immunodeficiency Virus
|
Like all viruses, human immunodeficiency virus reproduces using the genetic machinery of the cell it infects, usually a CD4+ lymphocyte.
Drugs used to treat HIV infection were developed based on the life cycle of HIV. These drugs inhibit the three enzymes that the virus uses to replicate or to attach to and enter cells. |
HIV also infects other cells, such as cells in the skin, brain, genital tract, heart, and kidneys, causing disease in those organs.
Recommended Reading: Zithromax Z Pak For Sinus Infection