Guidelines For Infection Control In The Special Subsets
Immunocompromised patients are those patients whose immune mechanisms are deficient because of immunologic disorders infection or congenital immune deficiency syndrome), chronic diseases , or immunosuppressive therapy . Immunocompromised patients who are identified as high-risk patients have the greatest risk of infection caused by airborne or waterborne microorganisms. Patients in this subset include persons who are severely neutropenic for prolonged periods of time of < 500 cells/mL), allogeneic HSCT patients and those who have received the most intensive chemotherapy .
In general, opportunistic infections result from at least 1 of 3 basic mechanisms: Exogenous acquisition of a particularly virulent pathogen , reactivation of an endogenous latent organism endogenous invasion of a normally commensal or saprophytic organism .
The post-transplant timetable can be divided into three time periods:
Hand hygiene
- The most important intervention is hand hygiene. When hands are visibly dirty, contaminated with proteinaceous material, or visibly soiled with blood or body fluids, wash hands with either a non-antimicrobial soap and water or an antimicrobial soap and water
- If hands are not visibly soiled, or after removing visible material with non-antimicrobial soap and water, the preferred method of hand decontamination is with an alcohol-based hand rub .
Isolation
Room ventilation
Cleaning
Protective clothing
Food and drink
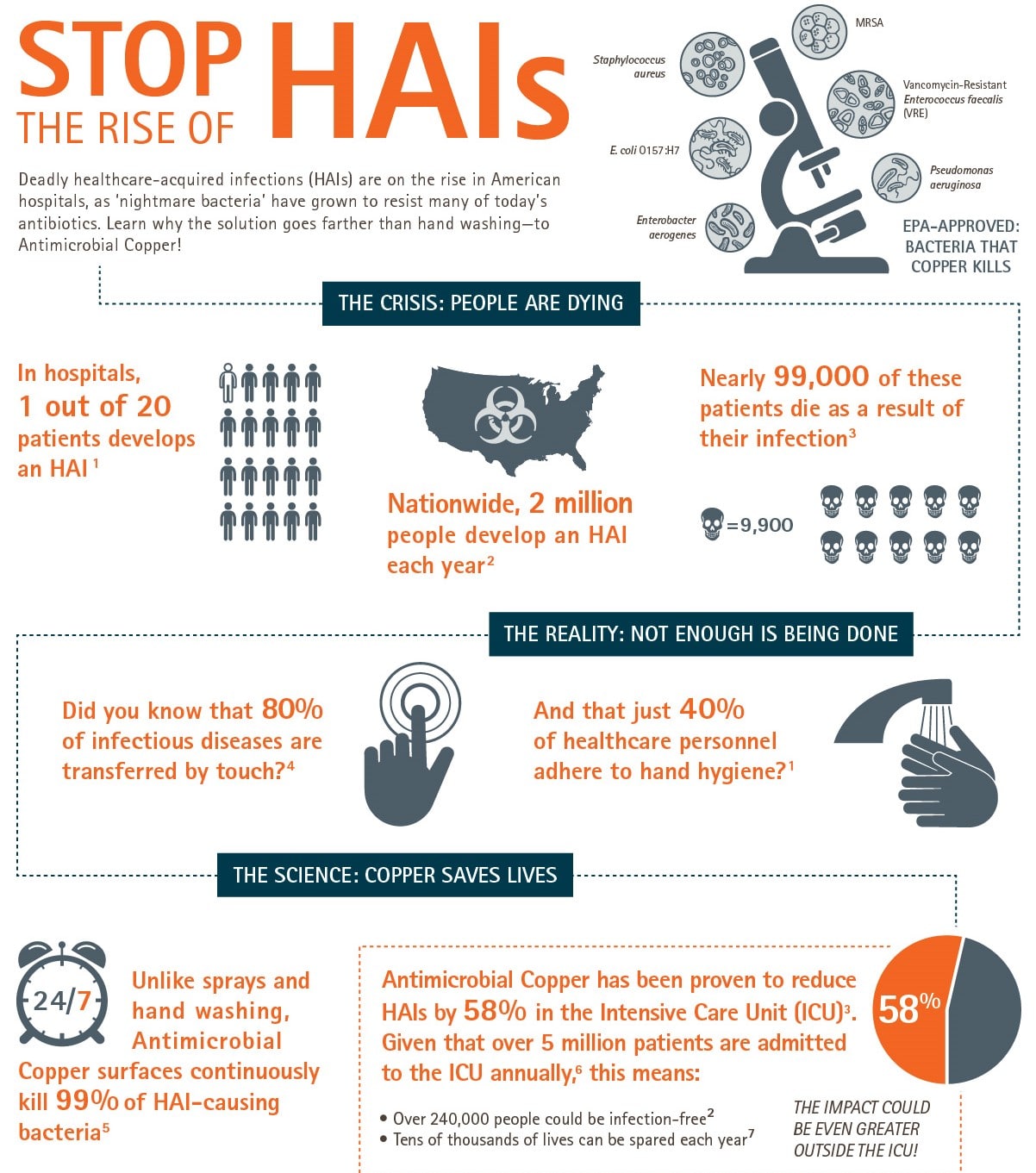
Why Is Hai Prevention So Important
Preventing hospital acquired infections is part of your responsibility to your patients, your co-workers, and yourself. Its an important part of keeping everyone healthy and safe.
HAI prevention practices can lead to an estimated $25-$31.5 billion in medical cost savings.2 Prevention saves hospitals money and allows medical professionals to focus on the primary condition of patients in their care.
Safe Management Of Equipment
It is essential any equipment you introduce into the healthcare facility is fit for purpose and intended for medical use. Where possible you should ensure the equipment comes with a robust service package and staff members are adequately trained on the safe use of this equipment.
Equipment can also be a known source of cross infection. For example, Oxford University Hospital traced an outbreak of a Hospital Acquired Infection, Canada Auris, back to their contact axilla thermometers.
Non-contact thermometers, such as the TRITEMP reduce touchpoints with customers, and require zero plastic probe covers, reducing the amount of contaminated waste, and optimising infection control.
With advances in technology, it is advisable when investing in new equipment for a hospital to ensure the equipment is optimised for infection control and prevention.
Does it eliminate the production of hazardous waste? Does it reduce contact? Can it be easily cleaned and decontaminated if it is to be used for multiple patients?
Also Check: How To Prescribe Diflucan For Yeast Infection
Why Dont People Always Wash Their Hands
Studies show that healthcare providers wash their hands less than ½ the times that they should.3 But why is this the case, if hand washing is so important to preventing healthcare associated infections?
One reason may be that healthcare workers may need to wash their hands as many as 100 times per 12 hour shift .3
One study found a variety of risk factors for poor adherence to recommended hand-washing practices including:4
| Observed |
|
The study recommends educating staff on hand washing guidelines and agents. It states that past studies found that alcohol-based hand rubs that contained emollients were less irritating to the skin than the soaps tested.4
One option for alcohol-based hand sanitizer is Antiseptic Bio-Hand Cleaner, which contains 67% ethyl alcohol and aloe vera.
Other hand sanitizer options include 3M Avagard D Instant Hand Antiseptic, which meets CDC, AORN, and WHO Guidelines and is compatible with CHG an 2XL Touch-Free Foam Hand Sanitizer a dermatologist-tested option with Vitamin E and Aloe to soothe dry and irritated skin.
What To Do If You Are Unhappy With Your Healthcare
If you have any questions, concerns or complaints about your condition or the care you are receiving please speak directly to your treating doctor or nursing staff as this is often the quickest and easiest way to resolve issues.
If you are unable to take your complaint to the health service provider directly or the issue is not resolved to your satisfaction, there is more you can do:
- take a look at Better Health Channels Complaints about health services page
Also Check: Genital Herpes Vs Yeast Infection
Who Is At Risk For A Nosocomial Infection
Factors that increase the risk for a include increasing age, length of hospitalization, excessive or improper use of broad-spectrum antibiotics, and the number of invasive devices and procedures :_Nursing” rel=”nofollow”> mechanical ventilation). In addition, most patients often have accompanying conditions such as , , , or malnutrition.
Join millions of students and clinicians who learn by Osmosis!
Less Than Half Of Hais Involve Devices Or Surgeries
A study from the New England Journal of Medicine found that device-associated infections made up 25.6% of all HAIs, while surgical-site infections accounted for 21.8% of HAIs. So, what caused the 52.6% of HAIs that were not associated with devices or operative procedures?One pathogen stands out. The bacterium Clostridioidesdifficile accounts for 12.1% of HAIs, notes the NEJM study. C. difficile is easily spread from person to person and caused an estimated 223,900 HAI cases and 12,800 deaths in 2017, according to the CDCs 2019 Antibiotic/Antimicrobial Resistance threat report. C. difficile is resistant to multiple antibiotics used in clinical settings, including aminoglycosides, lincomycin, tetracyclines, erythromycin, clindamycin, penicillin, cephalosporins, and fluoroquinolones, according to research from the Journal of Clinical Microbiology. Treatment with antimicrobials significantly increases the risk of developing a C. difficile infection.
Read Also: Do I Need Meds For A Sinus Infection
Cdc Checklist For Core Elements Of Hospital Antibiotic Stewardship Programs
The checklist is a companion to Core Elements of Hospital Antibiotic Stewardship Programs. This checklist should be used to systematically assess key elements and actions to ensure optimal antibiotic prescribing and limit overuse and misuse of antibiotics in hospitals. CDC recommends that all hospitals implement an Antibiotic Stewardship Program.
Catheter Associated Urinary Tract Infections
Among hospital-acquired urinary tract infections, 7080% are attributable to the use of an indwelling urinary catheter. Catheter-Associated Urinary Tract Infections are the most frequently observed conditions, with an incidence 40% of all HAIs .
The duration of catheterization is the most important risk factor for developing CAUTI. Therefore, reducing unnecessary catheter placement and minimizing the duration of catheter stay in situ are the main strategies for prevention of CAUTI. Additional risk factors include female sex, older age, diabetes mellitus, renal failure, and malnutrition .
Although the proportion of bacteremic individuals who develop symptomatic infection is low, given the high frequency of indwelling urinary catheter use, CAUTI is one of the most common causes of secondary bloodstream infection. CAUTI is the source of approximately 20% of healthcare-acquired bacteraemia episodes in acute care facilities and more than 50% in long-term care facilities .
The estimated cost of HAIs in a Polish Intensive Care Unit ranges from EUR 10,035 to 22,411. While in the USA, an estimate of 449,334 healthcare-associated CAUTIs per year, is associated with an additional cost of US$74910,077-9 per admission in 2007 .
Comprehensive recommendations have been published to assist acute care hospitals in implementing and prioritizing their CAUTI prevention efforts .
Also Check: Frequent Bladder Infections After Intercourse
What To Expect If You Get An Infection In Hospital
If you do get an infection in hospital, measures may be put in place to stop the spread of the infection to other patients.Depending on the type of infection, these measures might include:
- being moved to a single room with your own bathroom
- being nursed by staff wearing gloves and gowns
- being put last on the surgery list.
V Standard Procedures Or Standard Operating Procedures
1. The organization should have a well designed, comprehensive and coordinated infection control programme aimed atreducing / eliminating risks to patients, visitors and providers of care.2. The organization must have infection control manual, which should be periodically updated.3. The infection control team is responsible for surveillance activities in identified areas of the hospital.4. The organization should take actions to prevent, reduce the risk of Hospital Acquired Infections in patientsand employees.5. Proper facilities and adequate resources are to be provided to support the infection control programme.6. The organization must take appropriate actions to control outbreaks of infections.7. There should be documented procedures for sterilization activities in the organization.8. Statutory provisions with regard to Bio Medical Wastes should be complied with.9. The infection control programme has to be supported by the organizations management and should train staffs ofemployee health.
Recommended Reading: Can Minocycline Treat Tooth Infection
Our #1 Hai Prevention Tip: Hand Hygiene
Clean hands are a crucial part of preventing the spread of deadly germs and HAIs to patients as well as preventing healthcare providers from acquiring infections from patients. The CDCs Clean Hands Count campaign highlights this important infection prevention step.
Check out this video created by Toronto General Hospital on the importance of hand washing!
This video may seem a little silly, using green paint to visualize germs, but it also highlights an important point and allows you to see why hand washing matters. When we dont wash our hands, the germs spread and can lead to healthcare-associated infections.
Statewide Prevention And Reduction Of Clostridioides Difficile
![5 Strategies to Reduce Surgical Site Infection [INFOGRAPHIC] 5 Strategies to Reduce Surgical Site Infection [INFOGRAPHIC]](https://www.infectiontalk.net/wp-content/uploads/5-strategies-to-reduce-surgical-site-infection-infographic-medline.jpeg)
The Maryland Statewide Prevention and Reduction of Clostridioides difficile Collaborative is targeting C. difficile infections in acute care facilities in Maryland.Using expertise and resources available through the Maryland Prevention EpiCenters and the Maryland Department of Health, SPARC has been created to help hospitals implement customized interventions to enhance CDI prevention efforts. To learn more, click on the SPARC logo below.
Recommended Reading: Can A Yeast Infection Cause Bleeding
Preventing Healthcare Associated Infections
Healthcare workers use various well established procedures to help prevent infections, including:
- infection control procedures and policies
- correct and frequent hand hygiene measures by all staff and patients
- keeping the healthcare environment and equipment clean
- complying with standard sterile techniques when performing surgery, caring for wounds or inserting and caring for medical devices such as intravenous cannulas and urinary catheters
- using antibiotics appropriately to prevent and treat infections.
Hospitals will also participate in surveillance programs to monitor infection rates and measure the impact of infection prevention practices.
What Are The Most Important Facts To Know About Nosocomial Infections
are infections patients acquire while admitted to a health-care facility and generally develop 48 hours or later after admission. These infections can lead to serious problems like and even death. Most are preventable, with prevention guidelines set by national public health institutes such as the Centers for Disease Control and Prevention . The risk of developing a partially depends on how strictly health-care facilities follow infection control guidelines. Patients at increased risk of infection include those with comorbid conditions, increased age, recent treatment with antibiotics, and prolonged hospitalizations. The most common type of involves invasive devices and procedures :_Nursing” rel=”nofollow”> mechanical ventilation, or surgery).
Recommended Reading: Can You Do A Root Canal On An Infected Tooth
Hand Sanitizer Vs Soap And Water
The CDC recommends using alcohol-based hand sanitizer when your hands are not visibly dirty because it is potentially more effective at killing hand germs and less irritating and drying to your skin than soap. Plus, its easier to use during the course of care.3
A 2014 study on strategies to prevent healthcare associated infections recommended performing hand hygiene with an alcohol-based hand rub as well. However, the study recommended using an antimicrobial or nonantimicrobial soap when hands are visibly soiled and during norovirus or C. difficile outbreaks.6
Another study found that 100% hand-hygiene compliance using soap and water would take 16 hours of nursing time for a 24 hour shift. However, using alcoholic hand disinfection at the bedside to achieve 100% compliance requires only 3 hours.5
Actions For This Page
- There are things you can do before and during your stay in hospital that will help reduce the chance of you getting an infection.
- Common types of healthcare associated infections are those associated with chest infections, surgical wounds or the insertion of medical devices such as an intravenous drip, urinary catheter or wound drain.
- Some people are more susceptible to healthcare associated infections than others.
Also Check: Strongest Otc Yeast Infection Medicine
Types Of Healthcare Associated Infection
The most common types of infection acquired in hospitals are:
- bloodstream infection
- wound infection
Infections are treated with antibiotics and usually respond well. Occasionally, infections can be serious and life threatening. Some bacteria are hard to treat because they are resistant to standard antibiotics. These bacteria are sometimes called superbugs.Some examples of superbugs are:
- methicillin resistant Staphylococcus aureus often called golden staph or MRSA
- vancomycin resistant Enterococcus also referred to as VRE
- carbapenemase-producing Enterobacteriaceae also referred to as CPE.
Placement And Infection Assessment
Before admission into the healthcare facility, all patients must be assessed for infection risks, as well as throughout their time in care. This will inform decisions about treatment.
Patients who may present a particular cross-infection risk may include:
- Patients presenting with diarrhea, or vomiting
- Those with an unexplained fever
- Patients who are known to have been previously positive with a Multi-drug Resistant Organism
- For COVID identifiers, Public Health Agency cites, loss of taste or smell, fever, and a new persistent cough as primary symptoms
Recommended Reading: Yeast Infection Urge To Urinate
The Surveillance Of Hais In England
Surveillance involving data collection, analysis and feedback to clinicians is vital when attempting to detect HAIs. However, the latest National Audit Office report states that there has been little improvement in the information available on the incidence and cost of HAIs since the NAOs original report on hospital infection rates in 2000 .
This is partly due to inconsistency in policy. The original NAO report recommended that the voluntary Nosocomial Infection National Surveillance Scheme , instigated in 1996, be made mandatory. However, instead of this, a new approach was introduced in April 2001 with mandatory laboratory-based MRSA bloodstream infection surveillance.
In 2002 responsibility for HAI surveillance transferred to the Health Protection Agency, which continued mandatory trust-wide surveillance of MRSA bacteraemias, other specific organisms, and orthopaedic surgical site infections. However, had it developed the system to include specific areas such as bloodstream, surgical site, and urinary tract infections, this information could have been fed back to clinicians to influence practice. Instead, as the data is collected across whole hospital sites clinical staff cannot relate it to their particular specialties.
Respiratory And Cough Hygiene

Proper respiratory and cough hygiene practices aim to reduce the risk of cross-transmission of different respiratory illnesses and pathogens such as, influenzas or COVID-19.
- Cover nose and mouth with disposable tissues if coughing or blowing/wiping the nose
- Bin the tissue after use
- Ensure you wash your hands after
Healthcare professionals should both practice respiratory and cough hygiene themselves and encourage it among patients. Ensure there are tissues, plastic bags for the used tissues and handwashing stations.
Also Check: When To See A Doctor For Yeast Infection
What Is A Hai
HAI is an acronym that is used interchangeably for Hospital Acquired Infections and Healthcare Associated Infections. They are sometimes also referred to as nosocomial infections.
People get these infections while receiving care for other medical conditions. To be considered a HAI, the infection must not be present before that individual is under hospital care.
General Measures Of Infection Control
Isolation
There are two types of isolation in the ICU:
Isolation rooms should have tight-fitting doors, glass partitions for observation and both negative-pressure and positive-pressure ventilations.
Patient at risk of nosocomial infections
There are patient, therapy and environment related risk factors for the development of nosocomial infection.
- Age more than 70 years
- Drugs affecting the immune system
- Indwelling catheters
- Prolonged ICU stay .
Observe hand hygiene
Hands are the most common vehicle for transmission of organisms and hand hygiene is the single most effective means of preventing the horizontal transmission of infections among hospital patients and health care personnel.
When and why follow World Health Organizations five moments for hand hygiene
World Health Organization’s five moments for hand hygiene
Follow standard precautions
Standard precautions include prudent preventive measures to be used at all times, regardless of a patient’s infection status.
Gloves
Gown
Mask, eye protection/face shield
Shoe and head coverings
- They are not required for routine care .
Patient-care equipment
Airborne precautions
Don’t Miss: Fastest Way To Heal Yeast Infection
Whats In For Preventing Hospital Acquired Infections
A study entitled The Health Professional’s Role in Preventing Nosocomial Infections, declares that Frequent hand washing remains the single most important intervention in infection control.5 However, they also include other suggestions for practical ways to prevent HAIs.5
Whats In?
Why Is Infection Control So Important
Infection Control is becoming increasingly important in recent times as there has been a rise in the number of Hospital-Acquired Infections . WHO estimates that 7% of all patients admitted into healthcare facilities will acquire at least 1 HAI. In January 2021, NHS England estimated that 18% of COVID-19 cases were in fact hospital-acquired, and during the first wave of the pandemic, reports cited that 1 in 8 hospitalised COVID cases were as a result of infections acquired in the hospital.
To mitigate against any infection risks in hospitals, healthcare staff are advised to perform 10 Standard Infection Control Precautions . These Infection Control measures help to minimise the spread of both known and unknown pathogens. SICPs must be performed by all healthcare personnel, at all times and for all patients to mitigate against the risk of HAIs.
Also Check: Will Bactrim Treat A Sinus Infection