Clinical Landmarks For Terminating Primary Prophylaxis
After ART is initiated and HIV viremia is suppressed, PCP and toxoplasmosis prophylaxis should continue until the CD4 count exceeds 200 cells/L for 3 months or 100 to 200 cells/uL with negative HIV viral load for 6 months . Histoplasmosis prophylaxis can be discontinued when the CD4 count has exceeded 150 cells/L for 6 months coccidioidomycosis prophylaxis can be stopped when CD4 counts exceed 250 cells/L for 6 months and penicilliosis prophylaxis can be discontinued when CD4 counts exceed 100 cells/L for 6 months .
How Does Hiv Work
HIV is a virus that attacks CD4 cells . These white blood cells serve as helper cells for the immune system. CD4 cells send a biological SOS signal to other immune system cells to go on the offensive against infections.
When a person contracts HIV, the virus merges with their CD4 cells. The virus then hijacks and uses the CD4 cells to multiply. As a result, there are fewer CD4 cells to fight infections.
Healthcare providers use blood tests to identify how many CD4 cells are in the blood of someone who has HIV, as its one measure of the progression of HIV infection.
CDC refers to these as AIDS-defining conditions. If someone has one of these conditions, the HIV infection has advanced to stage 3 HIV , regardless of the number of CD4 cells in their blood.
Following are some of the more common opportunistic diseases. Becoming knowledgeable about these health risks is the first step in protecting against them.
What Are Opportunistic Infections
Opportunistic infections are infections that occur more frequently and are more severe in people with weakened immune systems, including people with HIV.
Many OIs are considered AIDS-defining conditions. That means if a person with HIV has one of these conditions, they are diagnosed with AIDS, the most serious stage of HIV infection.
OIs are less common now than they were in the early days of HIV and AIDS when there was no treatment. Todayâs HIV medicines reduce the amount of HIV in a personâs body and keep the immune system stronger and better able to fight off infections.
However, some people with HIV still develop OIs for reasons such as:
- they do not know they have HIV and so they are not on treatment
- they know they have HIV but are not taking ART
- they had HIV for a long time before they were diagnosed and so have a weakened immune system
- they are taking ART, but they have not yet achieved viral suppression
You May Like: Difference In Symptoms Between Uti And Yeast Infection
Progressive Multifocal Leukoencephalopathy In Hiv
Progressive Multifocal Leukoencephalopathy is an extremely serious viral disease of the brain. PML causes a quick decline in cognitive and motor functions of the body.
Symptoms vary and may include speech problems, weakness on one side of the body, loss of vision in one eye, or numbness in one arm or leg. PML is a late-stage disease that occurs only when the immune system is severely damaged.
Data Collection Tools And Procedures
Data were collected by face to face interviews by using a pre-tested questionnaire a pre-tested checklist to collect information regarding OIs and patients clinical records were reviewed. A pre-tested structured questionnaire was utilized to collect socio-demographic characteristics, another clinical information, and other risk factors. The questionnaires were pre-tested and validated before two weeks in the study time in Dore Bafana primary hospital on 5% of HIV positive patients who attend ART clinic which was outside of the study area and some modifications on sequence and arrangement of multiple answer questionnaire were made. Data collectors were five clinical nurses supervised by one BSC nurse supervisor and investigators. Training and practical demonstrations on interview techniques and document extraction procedures based on the checklist were given to data collectors for two consecutive days assessed for competency.
Dont Miss: External Vulvar Cream For Yeast Infection
Also Check: Best Treatment For Tooth Infection
Initial Tests And Prophylactic Regimens
On the patient’s first visit, serologies for syphilis hepatitis A, B, and C and toxoplasmosis should be obtained. Although the incidence of CMV disease, including retinopathy, has declined significantly, it is recommended that patients with HIV who are not at high risk for CMV infection be screened to confirm that they are CMV-negative . Such HIV-positive, CMV-negative persons would be instructed to limit exposure to CMV by using latex condoms and other barrier precautions , be informed of the risk for acquisition in daycare facilities , and be instructed to accept only CMV-seronegative or leukocyte-reduced blood products in nonemergent situations .
Preventing And Treating Ois
The best way to prevent OIs is to keep your immune system as strong as possible by taking HIV drugs as soon as you know that you are living with HIV. This allows the immune system to do its job of controlling infections.
If your CD4 cell count falls below 200, taking appropriate medications can prevent many OIs from developing. Taking medication to prevent disease is called “prophylaxis.” For example, the CDC recommends that people living with HIV whose CD4 counts are below 200 take a daily antibiotic or similar medication to avoid getting Pneumocystispneumonia ..
Effective treatment options are available for most OIs. The earlier you tell your health care provider about any symptoms, the sooner you can get diagnosed and treated, and the better your chances that the treatment will work and that you will recover fully. You may be able to stop prophylaxis or maintenance treatments if your CD4 cell count goes up and stays up. However, you should not stop any treatment without talking first to your health care provider.
Recommended Reading: How To Treat Yeast Infection Medication
What Are The Most Common Ois
In the early years of the AIDS epidemic, OIs caused a lot of sickness and deaths. Once people started taking strong antiretroviral therapy , however, a lot fewer people got OIs. Its not clear how many people with HIV will get a specific OI.
In women, health problems in the vaginal area may be early signs of HIV. These can include pelvic inflammatory disease and bacterial vaginosis, among others. See fact sheet 610 for more information.
The most common OIs are listed here, along with the disease they usually cause, and the CD4 cell count when the disease becomes active:
Opportunistic Infections In Hiv
Overview
Advances in antiretroviral therapy have made it possible for people with HIV to live longer and healthier lives. According to the Centers for Disease Control and Prevention , 1.1 million Americans were living with HIV at the end of 2015.
However incredible the advances in care, people who are HIV-positive still have an important role to play in safeguarding their health. They should work closely with their healthcare providers and stay on top of their antiretroviral therapy. They also need to protect themselves from opportunistic infections, which are a serious threat to anyone living with HIV.
Recommended Reading: Diflucan For Yeast Infection 1 Pill
Are Opportunistic Infections Common In People With Hiv
OIs are less common now than in the early days of HIV and AIDS when there was no treatment. Todays HIV medicines reduce the amount of HIV in a persons body and keep the immune system stronger and better able to fight off infections.
However, some people with HIV still develop OIs for reasons such as:
- they do not know they have HIV and so they are not on treatment
- they know they have HIV but are not taking ART
- they had HIV for a long time before they were diagnosed and so have a weakened immune system
- they are taking ART, but their drug combination is not working as expected and is not keeping their HIV levels low enough for their immune system to fight off infections
Recurrent Pneumonia In Hiv
Studies have shown that persons with HIV-related immunosuppression are at an increased risk of pneumonia, an infection of the lungs that can be caused by bacteria, viruses, or fungi. Symptoms include cough, often with mucous production, fever, chills, and difficult breathing. Streptococcus pneumoniae, also called Pneumococcus, can be prevented with a vaccine that all HIV-infected people should receive.
Recurrent episodes of pneumonia are more strongly associated with immunosuppression than are single episodes.
Patients with CD4 counts less 200 cells/mm3 may be at higher risk of recurrent episodes of pneumonia.
Don’t Miss: Sinus Infection When To See A Doctor
Am I More At Risk Of Covid
We are still learning about COVID-19. But current evidence suggests that people with HIV have an increased risk of becoming seriously ill or dying from it.
The best way to stay healthy is to properly take your HIV medication and any other medication you are on. It is also important to follow national guidelines on preventing COVID infections and testing, and get a COVID-19 vaccination.
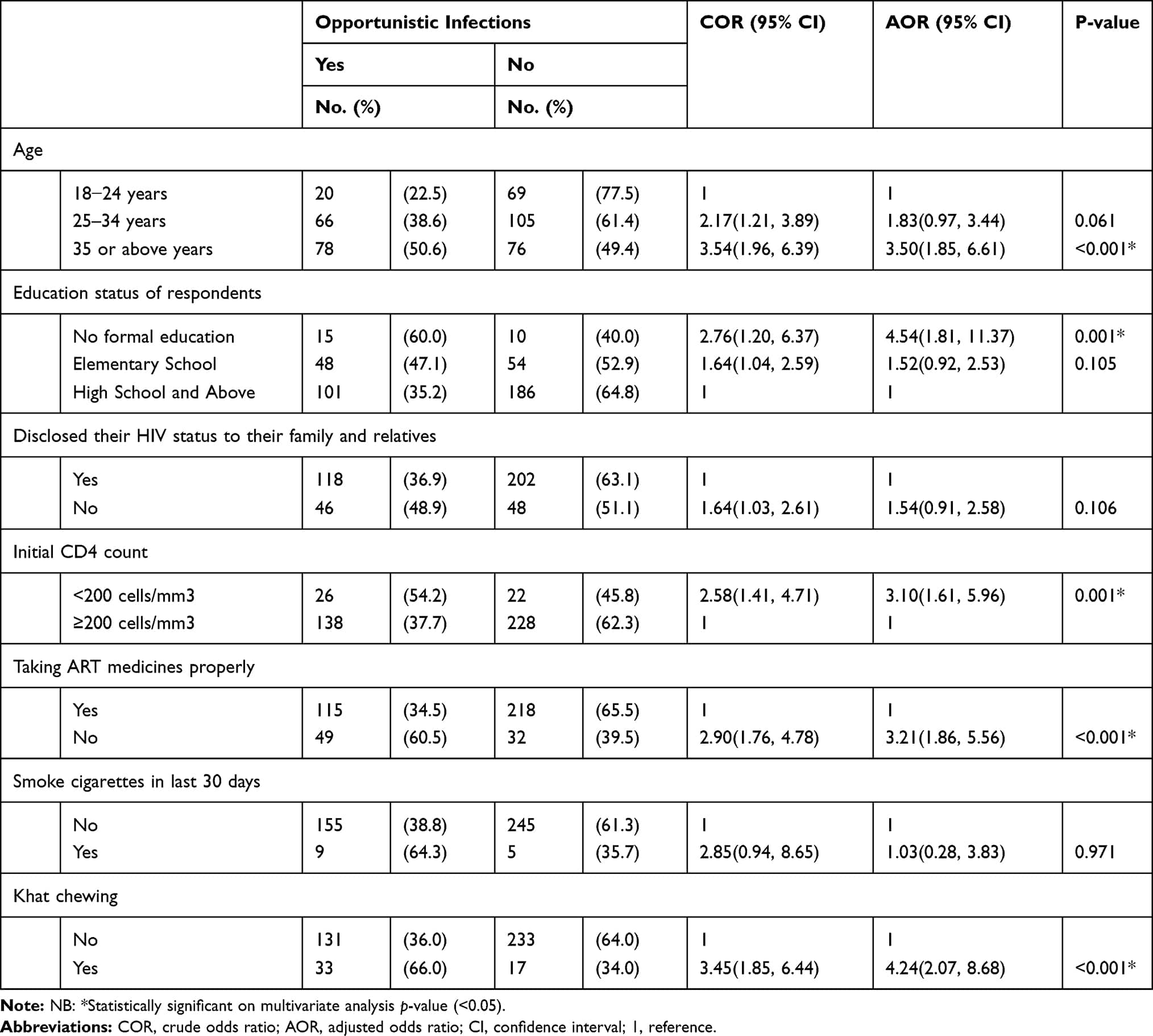
Environmental And Behavioral Related Characteristics
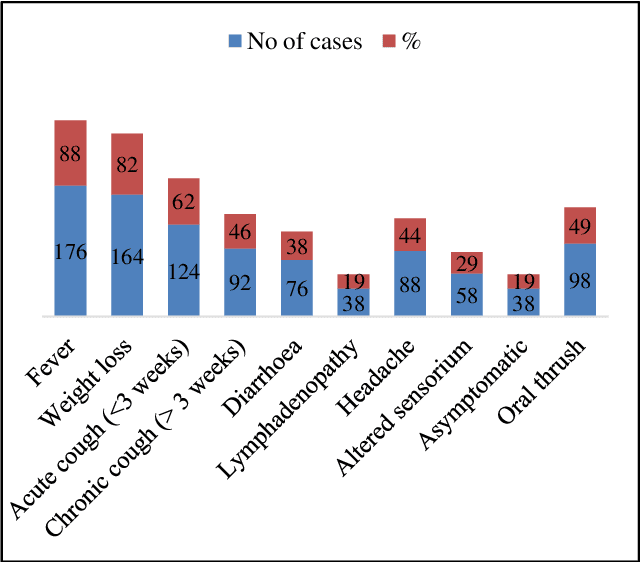
The majority of 273 were living in the cemented floor house. Most of 401 had a latrine, among this 395 were shared with their family and neighbors. More than half of 287 used Garbage can or sac to disposer refuse. The main source of drinking water was 398 pipe water. Regarding behavioral related factors, 27 were used any tobacco products, among this 14 were current cigarette smokers. The prevalence of Khat chewing was 48 . Regarding alcohol consumption, 71 were ever drunk alcohol, 63 were drinking alcohol in the last 30 days .
|
Table 2 Environmental and Behavioral Characteristics of HIV-Positive Adults on ART at Selected Hospitals in Sidama Regional State, Southern Ethiopia, 2019 |
Also Check: Can Prenatals Cause Yeast Infections
Common Opportunistic Clinical Manifestations In People With Hiv
In this section, we will be describing the clinical signs and symptoms associated with common opportunistic clinical manifestations that you may encounter in PLHIV during community visits, or at your health post. Where possible, we have included photographs showing typical clinical manifestations of an opportunistic disease in a PLHIV, so that you become familiar with them.
Identifying opportunistic infections and diseases will help your work in the context of PLHIV in two ways. First, you may be able to categorise patients in one of the four stages of the WHO HIV clinical staging. You will then be able to refer them to the nearest health centre for comprehensive HIV services, such as cotrimoxazole chemoprophylaxis , and for specific treatments for HIV/AIDS. In some cases, you will need to refer the person living with HIV urgently, whereas in others you will just need to reassure the patient, and/or treat minor ailments. Note that all conditions described below should be referred to the nearest health centre if they are clinical stage 2 and above, with increasing urgency the higher the WHO clinical stage.
Secondly, if staging has been carried out by a health worker at a health centre or hospital, you will be able to appreciate at what stage of the disease a person living with HIV is, and provide the best possible care for that patient.
21.4.1 Persistent generalised lymphadenopathy
Itching skin rash may be due to the following two conditions:
How Can Opportunistic Infections Be Prevented
As these infections only occur in people with a weakened immune system, the most important way to prevent them would be to treat the underlying HIV infection. Highly Active Antiretroviral Treatment is very effective at treating HIV and ensuring the virus is adequately suppressed. With a low or undetectable viral load, the bodys immune system has time to recover and when the CD4 cells have returned to sufficient numbers, the risk of Opportunistic Infections is lowered drastically. The earlier an HIV infection is diagnosed, the earlier treatment can be started and the better the chances of avoiding Opportunistic Infections.For patients who are diagnosed with HIV later and have low CD4 counts at diagnosis , it is important to consider Opportunistic Infections prophylaxis while we are waiting for HAART to work. This means starting patients on certain medications to prevent some of these specific infections. It may take 6-12 months for the CD4 counts to recover once HAART has been initiated once the CD4 counts are improved, these prophylactic medications may be stopped.Other general advice for people living with HIV would include:
- Reducing or preventing exposure to other sexually transmitted infections
- Getting vaccinated
- Avoiding undercooked or raw foods
- Avoid drinking untreated water
- Speak to your doctor about any other changes that may need to be made at home, work, or when on vacation to reduce exposure to OIs
Take Care!
Don’t Miss: Vitamin C For Yeast Infection
What Are Some Of The Most Common Opportunistic Infections
Some of the most common OIs in people with HIV are:
- Herpes simplex virus 1 infectionâa viral infection that can cause sores on the lips and mouth
- Salmonella infectionâa bacterial infection that affects the intestines
- Toxoplasmosisâa parasitic infection that can affect the brain
- Pneumocystis pneumonia âa lung infection caused by a fungus
- Tuberculosisâa bacterial infection that affects the lungs and can also affect other parts of the body such as the kidneys, brain, skin, lymph nodes, and eyes.
Visit CDC for a detailed list.
Fungal Or Yeast Infections
According to current NIH guidelines, Cryptococcus neoformans and Candida infections do not warrant primary prophylaxis. In the case of Cryptococcus infection, primary prophylaxis has not been shown effective in Thailand. New WHO guidelines recommend cryptococcal antigen testing and preemptive therapy in antigen-positive patients with a CD4 count < 100 cells/uL in Africa and other areas of high prevalence. Prolonged suppressive therapy for Candida is not recommended owing to risk of resistance. However, if necessary because of frequent recurrence or severe disease, fluconazole 100 mg PO thrice weekly for thrush , fluconazole 100-200 mg daily , or fluconazole 150 mg PO once weekly are the first recommended drugs.
Fortunately, aspergillosis and phycomycosis are rare in individuals infected with HIV. These infections should be considered in patients with invasive sinusitis and focal pulmonary lesions but do not warrant prophylaxis.
Travelers to malaria-prone areas should have malaria prophylaxis, and those who live in such areas should practice preventative measures, such as the use of treated mosquito netting.
Also Check: Embarrassed To Go To Doctor For Yeast Infection
What Can People With Hiv Do To Prevent Getting An Oi
For people with HIV, the best protection against OIs is to take HIV medicines every day.
People living with HIV can also take the following steps to reduce their risk of getting an OI.
Avoid contact with the germs that can cause OIs.
The germs that can cause OIs can spread in a variety of ways, including in body fluids or in feces. To avoid sexually transmitted diseases or infections, use condoms every time you have sex. If you inject drugs, do not share drug injection equipment. After any contact with human or animal feces, wash your hands thoroughly with warm, soapy water.
Ask your health care provider about other ways to avoid the germs that can cause OIs.
Be careful about what you eat and drink.
Food and water can be contaminated with OI-causing germs. To be safe, do not eat certain foods, including undercooked eggs, unpasteurized dairy products or fruit juices, or raw seed sprouts.
In addition, do not drink water directly from a lake or river. For more information, read the HIV and Nutrition and Food Safety fact sheet from HIVinfo.
Travel safely.
If you are visiting a country outside the United States, avoid eating food and drinking water that could make you sick. Before you travel, read the Centers for Disease Control and Prevention fact sheet on Traveling with HIV.
Get vaccinated.
Talk to your health care provider about which vaccines you need. To learn more, read the HIVinfo fact sheet on HIV and Immunizations.
Monitoring Of Treatment Response
Monitoring of response to treatment is done by assessing border activity and position. Photographic monitoring is helpful to detect subtle changes in the border that may indicate progression. Patients with low CD4+ T lymphocyte counts, positive blood CMV by PCR, and longer duration of AIDS are more likely to progress. With therapy, healing is generally expected in 4 to 6 weeks, although activity commonly recurs unless the underlying immunosuppression is effectively treated. Strategies for recurrence include reinduction, addition of foscarnet to ganciclovir, intravitreal injections, and implantation of the ganciclovir intraocular device. A recent review summarizes current treatment strategies for CMV retinitis.
Dont Miss: Is Hiv Curable Or Treatable
Read Also: Urinary Tract Infection Without Antibiotics
Hiv Symptoms In Children
Common symptoms due to HIV in a child can vary depending upon age . Most babies with HIV appear healthy at birth, but if the condition is left undiagnosed and untreated, signs or symptoms may appear within 2 to 3 months. The number of HIV-infected infants has remained steady at less than 200 new infant infections per year, according to CDC statistics. In 2018, 87 cases of HIV in children younger than 13 years of age were diagnosed in the United States.
| HIV Symptoms in Children | |
| Liver inflammation usually in children > 1 year old | |
| Complications due to chicken pox | Typically occurs in children > 1 year old |
Due to advances in treatment, children who are diagnosed and receive appropriate medical care and medications early in life can have similar positive outcomes as seen in adults. As with adults, antiretroviral therapy is a key component of managing symptoms, opportunistic infections, and reducing the risk of transmission.
Phases Of Hiv Infection
Clinical HIV infection undergoes 3 distinct phases: acute seroconversion, asymptomatic infection, and AIDS. Each is discussed below.
Acute seroconversion
Animal models show that Langerhans cells are the first cellular targets of HIV, which fuse with CD4+ lymphocytes and spread into deeper tissues. In humans, rapid occurrence of plasma viremia with widespread dissemination of the virus is observed 4 days to 11 days after mucosal entrance of the virus.
There is no fixed site of integration, but the virus tends to integrate in areas of active transcription, probably because these areas have more open chromatin and more easily accessible DNA. This greatly complicates eradication of the virus by the host, as latent proviral genomes can persist without being detected by the immune system and cannot be targeted by antivirals.
During this phase, the infection is established and a proviral reservoir is created. This reservoir consists of persistently infected cells, typically macrophages, and appears to steadily release virus. Some of the viral release replenishes the reservoir, and some goes on to produce more active infection.
The proviral reservoir, as measured by DNA polymerase chain reaction , seems to be incredibly stable. Although it does decline with aggressive antiviral therapy, the half-life is such that eradication is not a viable expectation.
Asymptomatic HIV infection
Read Also: How Long Does Hiv Fever Last
Read Also: Does Zpack Cause Yeast Infection