Predisposition To Infection: Neutropenia
Patients with neutropenia are predisposed to infection because of insufficient circulating neutrophils, lack of adequate myeloid marrow reserve, or congenital or acquired defects in neutrophil function . Neutropenia is frequently associated with mucosal or integumentary barrier disruption, and the indigenous colonizing florae are responsible for most infections. More than 20% of patients with chemotherapy-induced neutropenia develop skin and soft-tissue infections, many of which are due to hematogenous dissemination from other sites, such as the sinuses, lungs, and the alimentary tract . Important pathogens for neutropenic patients can be separated into organisms most likely to cause an initial infection and those more likely to cause a subsequent infection . Pathogens causing initial infections are usually bacteria, including both gram-negative and gram-positive organisms. Pathogens causing subsequent infections are usually antibiotic-resistant bacteria, yeast, or fungi .
Skin and soft-tissue infections in the immune compromised host: treatment and management.
How Is A Skin Infection Treated
Treatment depends on the cause of the infection and the severity. Some types of viral skin infections may improve on their own within days or weeks.
Bacterial infections are often treated with topical antibiotics applied directly to the skin or with oral antibiotics. If the strain of bacteria is resistant to treatment, treating the infection may require intravenous antibiotics administered in the hospital.
You can use over-the-counter antifungal sprays and creams to treat a fungal skin infection. If your condition doesnt improve, ask your doctor about prescription oral or topical creams. In addition, you can apply medicated creams to your skin to treat parasitic skin infections. Your doctor may also recommend medications to reduce discomfort like anti-inflammatory drugs.
Clinical Manifestations Of Inflammation
The cardinal manifestations of inflammation are warmth, erythema, edema, pain and dysfunction . Prolonged inflammation can lead to chronic edema, especially in the lower extremities, and can result in a postcellulitic syndrome. Ancillary systemic signs, such as fever, hypotension and tachycardia, result from cytokine-induced changes in thermoregulation and vascular resistance. The release of cytokines may be mediated by the normal immune cell function or by bacterial toxin stimulation. Out-of-proportion pain results from severe damage of the deep layers of skin produced by bacterial toxins, while bullous lesions are produced by toxin-mediated epidermal cleavage. Skin anesthesia, which may be present during the course of necrotizing fasciitis, occurs secondary to toxin-mediated nerve tissue damage. Also, violaceous lesions result from toxin-mediated lysis of erythrocytes and hemorrhage .
Read Also: What Do They Prescribe For Ear Infections
Are There Any Over
Over-the-counter oral antibiotics are not approved in the U.S. A bacterial infection is best treated with a prescription antibiotic that is specific for the type of bacteria causing the infection. Using a specific antibiotic will increase the chances that the infection is cured and help to prevent antibiotic resistance. In addition, a lab culture may need to be performed to pinpoint the bacteria and to help select the best antibiotic. Taking the wrong antibiotic — or not enough — may worsen the infection and prevent the antibiotic from working the next time.
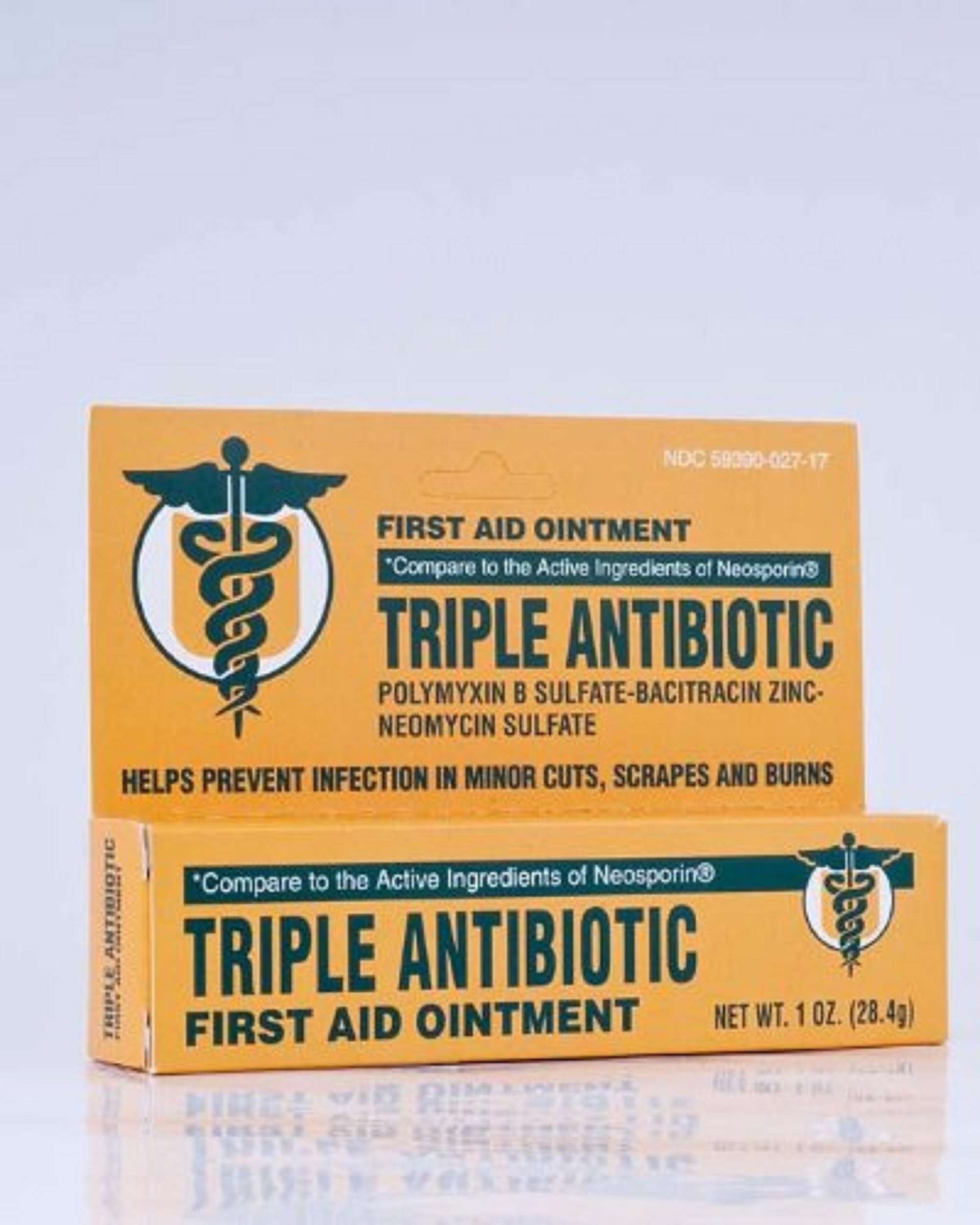
There are a few over-the-counter topical antibiotics that can be used on the skin. Some products treat or prevent minor cuts, scrapes or burns on the skin that may get infected with bacteria. These are available in creams, ointments, and even sprays.
Is Convenia A Broad Spectrum Antibiotic
Ten percent of all fines are redeemed with repentance. The solution must be used with 6 ml. Subcutaneous administration of the product is the most effective method. When it comes to bacteria, Convenia consists of cefovecin , which is a third generation cephalosporin with several different antibacterial properties.
Recommended Reading: Lupin 500 For Tooth Infection
Medications For Skin Conditions
Medications used to treat skin conditions include topical and oral drugs.
Some common topical treatments for skin conditions include:
Some common oral or injection treatments for skin conditions include:
- Antibiotics: Oral antibiotics are used to treat many skin conditions. Common antibiotics include dicloxacillin, erythromycin, and tetracycline.
- Antifungal agents: Oral antifungal drugs include fluconazole and itraconazole. These drugs can be used to treat more severe fungal infections. Terbinafine is an oral antifungal medicine that may be used to treat fungal infections of the nails.
- Antiviral agents: Common antiviral agents include acyclovir , famciclovir , and valacyclovir . Antiviral treatments are used for skin conditions including those related to herpes and shingles.
- Corticosteroids: These medications, including prednisone, can be helpful in treating skin conditions linked to autoimmune diseases including vasculitis and inflammatory diseases such as eczema. Dermatologists prefer topical steroids to avoid side effects however, short-term use of prednisone is sometimes necessary.
- Immunosuppressants: Immunosuppressants, such as azathioprine and methotrexate , can be used to treat conditions including severe cases of psoriasis and eczema.
Surgical Examination And Drainage
Urgent consultation with a surgeon should be sought in the setting of crepitus, circumferential cellulitis, necrotic-appearing skin , evolving bullae, rapidly evolving cellulitis, pain disproportional to physical examination findings, severe pain on passive movement, or other clinical concern for necrotizing fasciitis. Wong et al have developed a scoring tool to assist in the diagnosis of necrotizing fasciitis. Cellulitis associated with an abscess requires surgical drainage of the source of infection for adequate treatment.
Serious concern for necrotizing fasciitis and/or the presence of necrotic skin should prompt examination of the fascial planes by immediate computed tomographic imaging or surgical direct observation, which, in most cases, can be performed at the bedside by an experienced surgeon. Circumferential cellulitis may result in compartment syndrome, which may require surgical decompression. Measurement of compartment pressures may be helpful in diagnosis.
Also Check: Vaginal Yeast Infection That Wont Go Away
Cautions With Other Medicines
Some medicines can affect the way that flucloxacillin works and increase the chance of you having side effects.
Tell your doctor if you’re taking any of these medicines before you start flucloxacillin:
- methotrexate, an anti-inflammatory medicine for arthritis and similar conditions
- warfarin, a medicine to prevent blood clots
- other antibiotics
Tell your doctor if you’ve recently had, or are due to have, an oral typhoid vaccination. Flucloxacillin can make it less effective.
Swelling And Redness In Your Lower Legs May Not Require Treatment With Antibiotics
If one or both of your lower legs are swollen and red, visit your doctor to find out why. In most cases, if both of your lower legs are swollen and red at the same time, its not because of an infection. That means you dont need antibiotics.
There are many other reasons why your lower legs could be swollen and red. For instance, you could have varicose veins or a blood clot in your leg. You could have an allergy to something you touched, such as a detergent or soap. Leg swelling could even be a sign of heart disease.
Before prescribing an antibiotic, your doctor should talk to you and do any tests needed to rule out these problems. Even then, you should take antibiotics only if theres a clear sign of an infection like cellulitis. Thats a common skin infection that causes redness and swelling.
Read Also: Frequent Bladder Infections After Intercourse
How Do Doctors Treat Skin Infections
Skin infections are very common, especially those caused by bacteria. In order to treat a skin infection, doctors will use antibiotics or topical ointments. When it comes to treating a bacterial skin infection at home, you should take the following steps: Doctors can treat skin infections in a variety of ways. The most common treatment includes using topical antibiotics and/or oral antibiotics such as doxycycline and erythromycin to kill the bacteria causing the outbreak. Skin infections are an unpleasant experience. They can be caused by a number of things, from dirty fishing gear to a cut from a sharp object. But for the most common types of skin infections, doctors usually prescribe antibiotics and topical creams like neosporin. Antibiotics can help your body fight off the infection and topical creams will help the area heal faster and more effectively. There are a few ways to treat a bacterial skin infection. The most common way is to use a topical ointment to kill the bacteria and relieve symptoms. Another treatment includes using an oral antibiotic. The last method, which is just as effective, includes using an oral or topical cream containing antibiotics.
General Management Of Skin Infections
With antibiotic treatment, signs and symptoms of skin infections begin to improve after approximately 2 to 3 days. If your skin infection does not improve or gets worse , notify your doctor right away. If you are prescribed topical or oral antibiotics, be sure to finish the full course of antibiotics unless otherwise directed. Keep in mind that the length of treatment will differ depending on the type and severity of the infection. Lastly, as is true among all skin infections, you should keep the affected area or wound clean with good skin hygiene.
Related Content:
Don’t Miss: Do I Have A Kidney Infection Or Uti
Antibiotics Can Be Harmful
If you have an infection, antibiotics can save your life. But antibiotics can also be harmful if you take them when you dont need them. The more antibiotics you use, the less likely they are to work when you need them.
Antibiotics can cause side effects. Antibiotics that you take by mouth can cause upset stomach, vomiting, diarrhea, and vaginal yeast infections. They can also cause allergic reactions. These include rashes, swelling, itching, and trouble breathing. Side effects from antibiotics cause nearly 1 in 5 trips to the emergency department.
Antibiotic creams and ointments can slow the healing of wounds. And they can cause redness, swelling, blistering, draining, and itching.
Antibiotics can breed superbugs. More than half of all antibiotics used in the U.S. are not needed. Thats according to the Centers for Disease Control and Prevention. Taking antibiotics when you dont need them can breed superbugs. These are bacteria that are hard to kill. They can make it harder to get well and cause health problems. You can spread superbugs to other people.
Antibiotics can be a waste of money. Antibiotics that you take by mouth can cost from $8 to more than $200. Antibiotic creams and ointments can cost from $5 to more than $150. Plus, you may need to spend more on healthcare and treatments due to side effects and superbugs from antibiotics.
08/2016
People At Risk Of Bacterial Infections

Antibiotics may also be recommended for people who are more vulnerable to the harmful effects of infection. This may include:
- people aged over 75 years
- babies less than 72 hours old with a confirmed bacterial infection, or a higher than average risk of developing one
- people with heart failure
- people who have to take insulin to control their diabetes
- people with a weakened immune system either because of an underlying health condition such as HIV infection or as a side effect of certain treatments, such as chemotherapy
Also Check: Urgent Care Treat Yeast Infections
Top 4 Antibiotic Treatments For Internal Or Severe Infections
Hospitalized patients with more complicated or severe forms of infections are often prescribed one of the following four antibiotics. These infections can include deep soft-tissue infections, surgical infections, major abscesses, wound infections and burn patients.
Oftentimes a broad-spectrum antibiotic is used in conjunction with the following antibiotics. Most options below use intravenous methods of delivering antibiotics into the body. A picc line may be used for prolonged treatment.
1. Intravenous Vancomycin
Vancomycin is often called an antibiotic of last resort for MRSA, though resistance against it has been growing. Vancomycin requires IV administration into a vein and can occasionally have severe side effects. Duration of treatment can last weeks to months. Tissue penetration is variable and it has limited penetration into bone. Its often prescribed for pneumonia .
- Resistance: Some strains of MRSA are now becoming resistant to Vancomycin, with one strain called VRSA .
- Side Effects and Precautions: Serious side effects can include ringing in ears, diarrhea, and hearing problems. Like most antibiotics, it can cause secondary infections like thrush or yeast infections. Because this medication is eliminated through the kidneys, it could cause kidney problems in the elderly or those with impaired kidney function.
2. Oral or Intravenous Linezolid
See the skin infection above for more info.
3. Intravenous Daptomycin
4. Oral or Intravenous Clindamycin
Who Is At Risk For Skin Infections
You are at a higher risk for a skin infection if you:
- Have poor circulation
- Have an immune system disease, such as HIV/AIDS
- Have a weakened immune system because of chemotherapy or other medicines that suppress your immune system
- Have to stay in one position for a long time, such as if you are sick and have to stay in bed for a long time or you are paralyzed
- Have excessive skinfolds, which can happen if you have obesity
You May Like: Can A Dentist Work On An Infected Tooth
When To Seek Medical Care
See a doctor right away if your child is younger than 3 months old and has a fever of 100.4 °F or higher.
See a doctor if you have symptoms of cellulitis or abscess. Although most cases of cellulitis resolve quickly with treatment, some can spread to the lymph nodes and bloodstream and can become life-threatening.
This Months Column Discusses Common Bacterial Skin Infections And The Proper Forms And Dosages Of Treatment
We were unable to process your request. Please try again later. If you continue to have this issue please contact .
Numerous topical antiinfective products are available to your patients over-the-counter or by prescription. Not only can the active antiinfective agents differ among these products, but their pharmaceutical dosage form may as well. The indications for topical antiinfectives, including acne vulgaris, various fungal skin infections, or viral skin infections are too broad to discuss in this column. Discussed in this months column will be the treatment of common bacterial skin infections, including impetigo, with topical antiinfectives.
Labeling for the various topical antibiotics includes numerous potential uses, including furunculosis and ecthyma, although their benefit, as proven by controlled clinical trials, is limited. Dermatology references generally recommend topical antibiotics as an option of therapy for impetigo, superficial folliculitis, furunculosis , and minor abrasions. Treatment of other pyodermas, such as carbuncles, ecthyma, cellulitis or erysipelas, are best treated with systemic antibiotics.
Pharmaceutical dosage forms
Impetigo
| It is helpful to have an appreciation of the amount of cream or ointment needed to treat a specific infected area: 1 g of cream will cover about a 10 cm x 10 cm area of skin 1 g of ointment will cover an area 5%-10% larger. |
Additional uses of topical antibiotics
Don’t Miss: Can You Get A Bladder Infection From Antibiotics
Which Antibiotic Is Best For Staph Infection
antibioticsstaph infectionsantibioticsantibiotics
. Also asked, what antibiotics cover staph?
Antibiotics commonly prescribed to treat staph infections include certain cephalosporins, nafcillin or related antibiotics, sulfa drugs, or vancomycin. Vancomycin increasingly is required to treat serious staph infections because so many strains of staph bacteria have become resistant to other traditional medicines.
Also, is amoxicillin good for staph infection? Penicillins with a beta-lactamase-inhibitor such as amoxicillin + clavulonic acid may be used to treat Staph. aureus infections and are sometimes effective against bacteria resistant to flucloxacillin.
Furthermore, how do you get rid of a staph infection fast?
How do you treat a staph infection at home?
Most small staph skin infections can be treated at home:
How To Take It
Swallow flucloxacillin capsules whole with a drink of water. Do not chew or break them.
It’s best to take flucloxacillin on an empty stomach. That means taking it at least 30 to 60 minutes before a meal or snack, or at least 2 hours after.
Liquid flucloxacillin is available for children, and people who find it difficult to swallow capsules.
If you or your child are taking liquid flucloxacillin, it will usually be made up for you by your pharmacist. The medicine will come with a syringe or spoon to help you take the right amount. If you do not have a syringe or spoon, ask your pharmacist for one. Do not use a kitchen teaspoon because it will not measure the right amount.
Don’t Miss: Will Vagisil Help Yeast Infection
Top 5 Mrsa Antibiotic Therapies For Skin Infections
MRSA is now resistant to many types of antibiotics.
Below are the five commonly prescribed antibiotics for MRSA skin infections, which are commonly picked up in communities as community type MRSA or CA-MRSA.
1. Clindamycin
It has been successfully and widely used for the treatment of soft tissue and skin infections as well as bone, joint and abscesses caused by Staph and MRSA. MRSA is becoming increasingly resistant to clindamycin in the United States.
- Resistance: MRSA is becoming increasingly resistant to clindamycin in the United States.
- Side Effects and Precautions: Diarrhea is the most common side effect, and it can promote C. difficile overgrowth infections in the colon. C. difficile infections appear to occur more frequently with clindamycin than other antibiotics. Other side-effects are pseudomembranous colitis, nausea, vomiting, abdominal cramps, skin rashes and more.
2. Linezolid
Folliculitis is a common type of MRSA skin infection often treated with oral antibiotics.
Approved for use in the year 2000, Linezolid is FDA approved for treating soft tissue and skin infections, including those caused by MRSA. It is often prescribed for CA-MRSA pneumonia and in particular, HA-MRSA pneumonia. Its commonly prescribed to people of all ages and is one of the most expensive treatment options, for a single course costing upwards of $1-2,000 for 20 tablets.
3. Mupirocin
4. Trimethoprim-Sulfamethoxazole
5. Tetracyclines