How Are Root Canal Infections Diagnosed
Dr. Nerness will first want to know the history of your symptoms. Dr. Nerness will usually take an x-ray of the tooth to evaluate the crown, roots, root canals, and supporting bone. In certain cases, a dental CT may be necessary to determine the extent of the infection. Since early root canal infections may not show up on the x-ray, Dr. Nerness will also complete a thorough examination of your teeth to evaluate for signs of infection.
What Are The Signs And Symptoms Of An Abscessed Tooth
It is also important to note that abscessed teeth may not have any symptoms at all. Because the tooth has lost vitality , there may be no pain associated with it. However, the abscess is still present and could be further spreading the dental infection. On occasion, an abscessed tooth is detected during a routine radiographic exam where the patient has not experienced any telltale symptoms of an abscessed tooth.
How Painful Is A Root Canal
Since qualified dentists and endodontists apply anesthesia to your problem tooth, you will experience no pain during the procedure however, your tooth may feel sensitive a few days after therapy, especially if it was painful and infected before the visit. Though this discomfort can be eliminated with convenient painkillers, you should approach your endodontist if pain is still present after several days.
Also Check: Strongest Antibiotic For Tooth Infection
The Main Causes Of Root Canal Infections
You might be surprised to learn that sometimes, people have root canal system infections without experiencing any signs or symptoms. In other cases, however, they have likely been disregarding the indicators for some time. After all, root canal system infections dont just happen overnightthey take time to take root. But how do they start?
What Are The Alternatives To Endodontic Retreatment And Endodontic Surgery
An untreated failed root canal is a severe infection. It can form a painful and dangerous abscess, and in some cases, even lead to a When it comes to infected pulp tissue, if you choose not to have endodontic retreatment or surgery, your only option is to extract the infected tooth. Though its preferable to keep your original tooth, if possible, an extraction followed by an implant is sometimes the only appropriate course of action.
Once your dentist extracts the tooth, your best choice is to have a dental implant that will mimic the look and feel of your natural tooth. Depending on the tooth, the cost of a dental implant is between $1,500 and $6,000. Additionally, the extraction itself can cost $50-900per tooth.
Also Check: Best Antibiotic For Severe Sinus Infection
B Having Symptoms Doesnt Always Indicate Endodontic Failure
Its possible that the symptoms youve noticed are not associated with your tooths root canal work per se. Here are some possibilities:
1) Referred pain
The nerve that services a tooth will have the duties of servicing other teeth and structures too. And its possible that a dental or medical problem associated with one of them may cause sensations that just happen to feel like theyre coming from your root canalled tooth.
2) Persistent Dentoalveolar Pain disorder
PDAP disorder is a relatively new term used to label situations characterized by this set of events:
- Pain associated with a tooth signals its need for root canal therapy.
- But following its treatment, the patient continues to experience discomfort with the tooth, for months on end.
- On evaluation, nothing can be found at fault with the tooth or the endodontic treatment it has received.
PDAP cases can be especially problematic, and difficult for a person to endure. For instance, it often takes a dentist some time to finally arrive at this diagnosis. And even then, possibly only after subjecting the tooth, or even neighboring teeth, to dental procedures that have no chance in providing a solution.
And since the underlying cause of PDAP disorder is unknown, treating it is unpredictable. Complete resolution of the patients pain may not be possible.
Weve given our coverage of this condition its own page. You can find it here: Persistent dentoalveolar pain disorder. PDAP
3) Tempromandibular joint disorder
Answer: Why Old Root Canals Can Start Hurting Again
Teeth that have already been treated with root canal therapy can at times become reinfected due to a variety of reasons. One of the more common causes is simply time, with time the materials used to seal the canal system can break down and fail, creating a potential space in which bacteria may possibly enter again and re-colonize leading to a re-occuring infection of the same tooth. Regardless of the reason of re-occuring infection or pain, if the tooth is mostly intact and has a good prognosis of further survival, re-treatment of the tooth with another root canal therapy is indicated. Keep in mind whenever re-treatment is performed, the prognosis is poorer for the tooth the second time around. As such, careful consideration should be made on whether to re-treat an already root canal treated tooth or perhaps consider completely replacing the tooth if the prognostic factors and chance of success of a re-treatment seem to be low. Only your doctor can make this assessment and you should speak about all your options with your treating doctor. Good luck!
Read Also: Can You Give Yourself A Yeast Infection
Why Would Someone Need A Root Canal
The reason someone would need a root canal performed on one or more of their teeth is because the soft tissue inside the tooth is either inflamed or infected. Some of the more common reasons someones tooth is inflamed or infected include a serious amount of decay on the tooth, a severe crack or severe chip in the tooth, a dental crown that is not working properly and having many procedures performed on one particular tooth. While some people would prefer to have their tooth pulled vs. getting a root canal performed, it is always recommended to keep ones natural teeth for as long as absolutely possible.
What Are The Symptoms Of An Infected Root Canal
Some signs and symptoms can be indicative of infection in the site of a root canal. Even if the root canal procedure was done some time in the past, there is still a chance of infection developing, especially if good oral habits have not been practiced by the person.
Pain. When there is pain in any part of the body, it can be a clear sign that something is not right. Pain can be a sign that there is infection inside the tooth that has a root canal
Swelling of the gumline. An infection inside a root canal can affect the gumline. There can be swelling and tenderness to the gumline when the inside of the root canal is infected. In most cases of swelling and tenderness, it is mostly localized to the area of the affected tooth, this is how you can be certain that an infection in the root canal is the cause.
Dental abscess. A dental abscess can cause extreme pain. There might have been some infected dental pulp that was left inside the tooth by accident, and this is what is causing the abscess in the affected tooth with the root canal.
Darkening of the tooth. The color of the tooth may be affected if there is an infection inside it. The color may change to a dark yellow or brownish color.
Chronic bad breath. Bad breath that does not go away, even after brushing is another sign that the affected tooth may be rotting from the inside.
Recommended Reading: Does Kidney Infection Go Away By Itself
Gum Tenderness And Swelling
Here are some swelling symptoms that may point to root canal infections:
- Swelling that lasts for a long period of time
- A gum pimple-like boil situated in front of or on the root tip
- The tooth that feels a bit taller than adjacent teeth
- A recurring pimple that forms on the gums
- Pronounced swelling.
Treatment Of Root Canal Re
Your dentist will investigate more to confirm the source of the pain. An X-ray will be the most useful tool here. It can be a small X-ray film placed in the mouth or a big X-ray machine to see more detail in a 3-dimensional view.
Besides, the dentist will likely find out the reason for the re-infection after the root canal. The reasons can be grouped into three categories:
Don’t Miss: What To Do If Infected With Ransomware
What Causes A Root Canal Infection
A root canal infection can occur for several reasons, though the basic root of the problem is always the penetration of bacteria into the pulp. Reasons for root canal infections are determined by the way the bacteria invades the tooth pulp. In this paragraph, we list the main causes of such an infection. The reasons for root canal infection include:
- Dental decay that allows bacteria to penetrate into the pulp and infect it.
- A cracked or damaged tooth, which opens the way for bacteria.
- An avulsed tooth that allows bacteria to penetrate into the pulp.
- Various tooth displacements caused by extrusion, intrusion, or subluxation.
- Sterile necrosis caused by tooth concussion .
- Tooth anatomy abnormality that allows bacteria to infect pulp tissue.
- Repeated dental treatments on the same tooth.
According to our experience, the main reason for a root canal infection is the caries that damages the tooth and allows bacteria to access and infect the pulp. This is why it is important to timely identify and eliminate caries in order to prevent pulp infections.
How Often Do Root Canals Fail

Out of the whopping 15 million root canals that are given every year which equals 41,000 performed every day in the United States an impressive 89% of those patients report being satisfied with the work their endodontists do. Multiple studies have been done to assess the success rate of the initial root canal. One study published in ISRN Dentistry determined that endodontic treatment is successful in 86% of cases.
However, success rates can vary based on the type of oral health professional who does the treatment. For example, one 2004 study found that root canal treatment was successful 98.1% of the time when endodontists perform it, but only 89.7% successful when general dentists perform it. Overall, root canal treatment is successful, approximately 90% of the time.
You May Like: Home Antibiotics For Tooth Infection
A How Can You Tell If Your Root Canalled Tooth Has A Problem
Many of the signs and symptoms of failed or failing root canal therapy are the same ones as those that originally signaled the tooths need for treatment. What to look for. In brief, here are some of the things you may notice:
1) Sensitivity to pressure
- The discomfort noticed might range from just slight tenderness to outright pain.
- It may be felt when biting/closing your teeth together, tapping on your tooth or directing forces to the tooth from the side .
The cause.
Typically this type of sensitivity is a sign of inflammation in the tissues that surround the tooths root.
The general scenario.
- Most cases of root canal treatment failure involve a situation where infection has reestablished itself inside the tooth.
- Microorganisms and infection byproducts that leak out of the tooth trigger an inflammation reaction in the tissues surrounding its root. Its the symptoms associated with this process, in these tissues external to the tooth, that result in its sensitivity to percussion.
2) Swelling.
Since failed endodontic cases typically do involve the presence of infection, swelling is often observed.
A persistent gum boil can be a sign of infection associated with failed root canal therapy.
Variants.
This page provides more detailed coverage about these lesions: What is a sinus tract? Pictures | Diagrams
3) Thermal sensitivity.
This symptom isnt as characteristic for failed endodontic work as pain and swelling. But experiencing it is a possibility.
Text And History Demonstrate Cawthorn Cant Evade Accountability For January 6
Root canals are a pretty common dental procedure. According to the American Association of Endodontists, over 15 million root canals are done every year in the United States alone.
But should you be concerned about a root canal infection? And are there any possible complications after a root canal you should know about?
Lets get into how to recognize a root canal infection, what causes them, and how theyre treated.
Don’t Miss: Can An Infection In Your Tooth Spread
What Causes An Abscessed Tooth
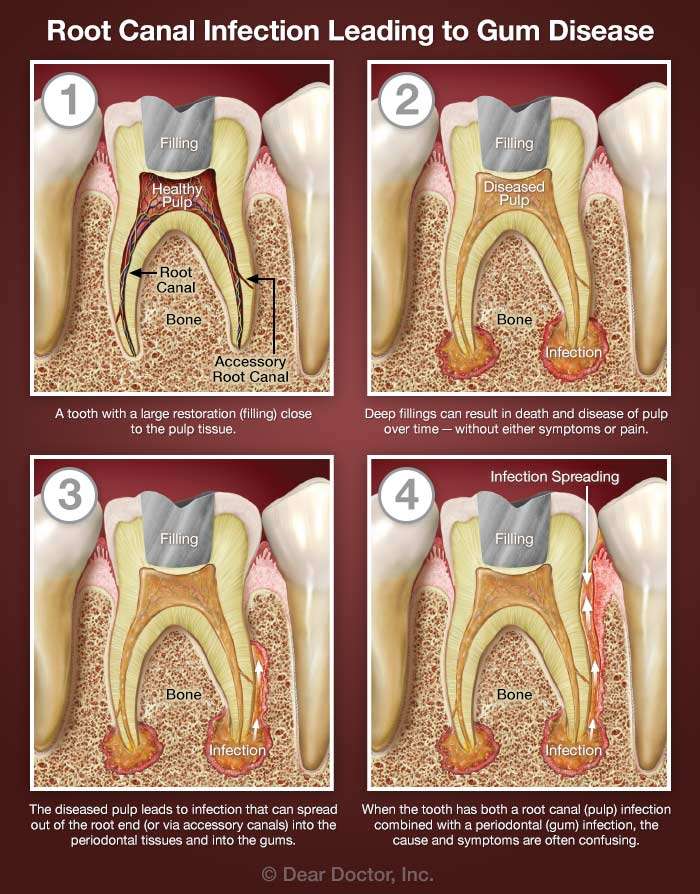
There are many causes for a dental abscess. A very common cause is when a dental cavity becomes so large and deep that it reaches the pulp chamber. An inflammatory process takes place within the tooth. Inflammation of the pulp is usually what is felt as a toothache. Pulpitis is further characterized by tests done by a dentist as reversible or irreversible. Reversible pulpitis means that the pulp is irritated but has an opportunity to recover. Irreversible pulpitis means that it will not recover, and the pulp is dying. Once the pulp is dead , an abscess can form as the infection spreads from the tooth to the gum ligament and jawbone below. Often, a tooth that becomes necrotic can still be saved if steps are taken to resolve the infection at an early stage.
Other causes for a tooth to become necrotic and abscess are a blow to a tooth, dental treatment such as a crown or a filling that gets too close to the pulp chamber, or trauma to a tooth from grinding or clenching. In every form of a tooth abscess, the pulp is adversely affected and is unable to recover from the insult or injury. A blow to the tooth can immediately sever the tooth’s blood supply. When the blood supply is lost, the nutrient supply is also lost. As a result, the pulp quickly dies. Trauma from grinding or clenching is a slower, progressive injury to a tooth.
So Whats The Treatment For Infected Root Canal Teeth
There are only 3 choices once an old root canal infection is diagnosed:
- Do nothing and just monitor or watch the progress of the infection
- Retreat or redo the root canal
- Extract the tooth and replace it
The first choice is not a very good one in my opinion, as you are leaving infection that drains endotoxins into your body. Endotoxins are byproducts of bacteria that cause inflammation locally and in your body as they affect your immune system. Keep in mind that these infections are 24/7 and cause stress on your immune system, sometime for years before they are discovered and treated.
The second choice of retreating the root canal can sometimes be done, although every time you redo a root canal the tooth becomes weaker and the root canal will fail faster the second time. I am of the opinion that when an existing root canal fails, the tooth should be extracted and replaced. However, Dr Val Kanter, a board certified endodontist in Beverly Hills, feels that a root canal can be retreated once with good results. Dr Kanter is an expert in biological and regenerative root canal therapies. She and I use ozone and a laser in our practice to treat root canal infections.
Also Check: How To Pull Out An Infected Tooth At Home
Recurrence Of An Infection
Two seals are placed in a root canal. One is the inner seal called the gutta percha. Another seal or crown is done on the outer part of the tooth. These seals can withstand tremendous abuse but are not immune to erosion. When one or both seals fail, bacteria might repopulate and cause an infection again. Proper care defines the longevity and effectivity of the seals.
C Not All Problem Teeth Display Symptoms You Can Detect
Usually what the dentist has discovered is referred to as a radiolucency Why these form., like the one shown in our illustration.
The grey area of treatment success.
The point that a tooths work might be classified as a failure even though it remains asymptomatic brings up the issue of tooth survival vs. case success.
In endodontic terms, survival refers to a lack of symptoms while success is associated with the more rigorous standard of both an absence of symptoms and evidence of periradicular tissue healing .
Read Also: Amoxicillin Vs Penicillin For Tooth Infection
Answer: Why Is My Old Root Canal Now Hurting Me
There are several reasons. The first of which is that the root canal treatment may be failing and need retreatment or possibly a minor surgery to save the tooth. Root canals are very successful, exceeding 90% today.Another reason is that the tooth may have cracked under the crown…you did have a crown done over the root canal tooth, didn’t you? Most root canal teeth do need restorations that are stronger than just fillings to strengthen the weaker root canal tooth. Root canaled teeth fracture easier and more frequently non-root canal teeth.A third reason is that you may have a gum problem or periodontal abscess around that tooth, that has no relationship to the root canal treatment.A fourth reason is that you may have had some movement of your teeth and you are hitting harder on the root canal tooth than the others.OK, you got the run down of possibilities. What did your dentist say after the x-ray and he examined your tooth? If he can’t give you an answer, then suggest you have your tooth evaluated by an endodontist .