Remote Control And Alarms
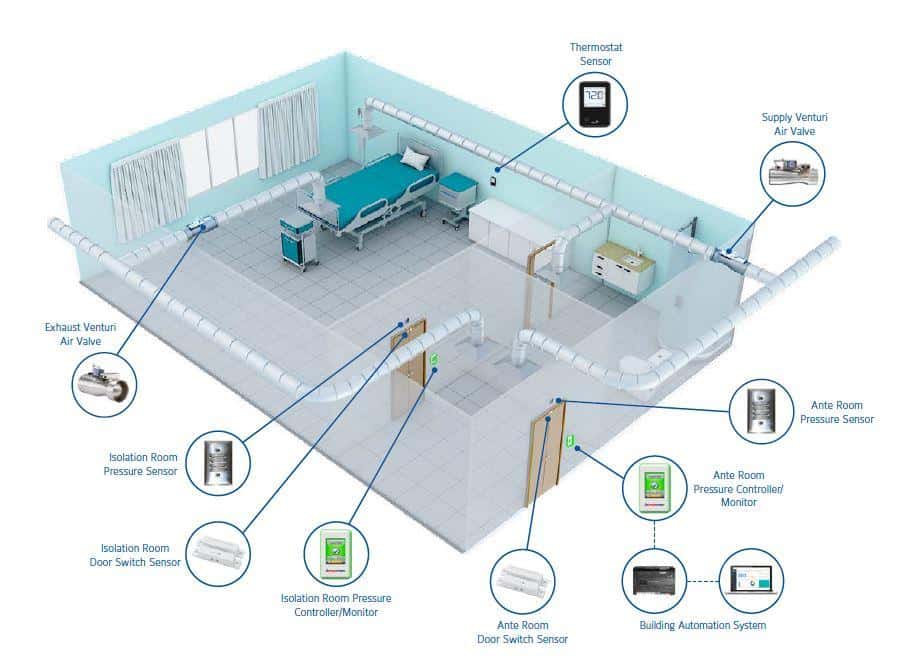
Medical staff can monitor and adjust the conditions of the rooms in real time via a user friendly supervisory panel that shows the overview of all the room within the department. The medical staff can monitor and change pressure mode, temperature and airflow rates. Thanks to the panel by the door of each room the environment can be monitored individually as well. The panels display a range of alarms to inform medical staff about unusual events in the room and enable a quick response.
Respiratory Hygiene/ Cough Etiquette
A combination of measures designed to minimize the transmission of respiratory pathogens via droplet or airborne routes in healthcare settings. The components of respiratory hygiene/cough etiquette are
These measures are targeted to all patients with symptoms of respiratory infection and their accompanying family members or friends beginning at the point of initial encounter with a healthcare setting 126
Quick Install Isolation Rooms
PortaFab Modular Building Systems are an ideal solution for quickly creating temporary, semi-permanent, and permanent isolation rooms within hospitals and medical centers. As a Clean Build alternative to traditional construction, PortaFabs pre-engineered systems require minimal onsite cutting and fabricating which minimizes contamination threats and helps comply with Class IV ICRA guidelines.
Quick Install
Recommended Reading: Olive Leaf For Tooth Infection
Ventilation Specifications For Health
The following tables from the AIA Guidelines for Design and Construction of Hospitals and Health-Care Facilities, 2001 are reprinted with permission of the American Institute of Architects and the publisher .120
Note: This table is Table 7.2 in the AIA guidelines, 2001 edition. Superscripts used in this table refer to notes following the table.
Table B2 Ventilation Requirements For Areas Affecting Patient Care In Hospitals And Outpatient Facilities1
The format of this section was changed to improve readability and accessibility. The content is unchanged.
Notes:
Appendix I:
Recommended Reading: How To Cure A Bacterial Sinus Infection
Additional Precautions Performing Aerosol
- Some procedures performed on patient with known or suspected COVID-19 could generate infectious aerosols. In particular, procedures that are likely to induce coughing should be performed cautiously and avoided if possible.
- If performed, the following should occur:
- HCP in the isolation room should wear an N95 or higher-level respirator, eye protection, gloves, and a gown, and ensure negative pressure is being maintained at all times via a visual indicator displaying negative pressure values.
- The number of HCP present during the procedure should be limited to only those essential for patient care and procedure support. Visitors should not be present for the procedure.
- AGPs should ideally take place in an AIIR.
- Clean and disinfect procedure room surfaces promptly as described in the section on environmental infection control below.
Expedient Patient Isolation Rooms
Oftentimes, local and national protective guidance issued during a pandemic might call upon the use of airborne infection isolation rooms for patients and/or specific patient procedures. Within U.S. hospitals, AIIRs are patient rooms with specific engineered features, intended to isolate and more-quickly remove potentially infectious patient aerosols. During an epidemic or pandemic, the demand for AIIRs may exceed their availability. When this occurs, healthcare facilities may choose to use portable fan systems with high-efficiency particulate air filtration to establish surge AIIR capacity. Although there is substantial research indicating potential shortcomings when HEPA fan/filter units are deployed incorrectly, there has historically been minimal guidance on how to deploy these units correctly. The National Institute for Occupational Safety and Health has developed guidance for using portable HEPA filtration systems to create expedient patient isolation rooms. The Expedient Patient Isolation Room guidance is researched based and is an effective solution for surge isolation capacity during outbreaks when traditional airborne isolation rooms are not available.
Figure 1. Research diagram of an example expedient patient isolation room for 2-bed patient room.
Read Also: Hiv Infected Healthcare Workers In New York State
How To Convert A Patient Room Into An Airborne Infection Isolation Room
The ongoing Covid-19 pandemic has created a demand on the US healthcare system which has not been experienced in many years, creating an overwhelming need for Airborne Infection Isolation Rooms . Most hospitals have a limited quantity of AIIRs available and these are typically filled by the normal caseload of illness.
In the hardest-hit areas of the country, some hospitals must quickly create additional AIIRs to handle the significant influx of patients diagnosed with COVID-19. Higgins and Associates has been working with several of our hospital clients to quickly and effectively facilitate the conversion of applicable normal patient rooms to AIIRs using guidelines that have been established by the CDC.
The CDC recommends that:
-
AIIRs are single-patient rooms at negative pressure relative to the surrounding areas, and with a minimum of 6 air changes per hour .
-
Air from these rooms should be exhausted directly to the outside or be filtered through a high-efficiency particulate air filter directly before re-circulation.
This CDC option allows the use of portable HEPA filtration unit to increase the air changes per hour within a normal patient room to more than 12 ACH. Portable room-air re-circulation units have been demonstrated to be effective in removing bioaerosols and aerosolized particles from room air.
The CDC states that “portable HEPA filtration units should be designed to:
Achieve 12 equivalent ACH
What Is An Airborne Infection Isolation Room
Also known as negative pressure isolation rooms, airborne infection isolation rooms are used by patients for hospitals and medical centers to prevent cross-contaminations and airborne infections from spreading throughout the facility.
These rooms are commonly recommended by the Center for Disease Control and Prevention to help protect the public from diseases and infections that spread easily like tuberculosis, measles, and the coronavirus .
- Central or point-of-use HEPA filters capable of removing particles 0.3 m in diameter for supply air
- Well-sealed rooms
- – Proper construction of windows, doors, and intake and exhaust ports
- – Smooth, cleanable ceiling tiles
- – Walls sealed above and below the ceiling
Pre-engineered systems can be assembled quickly with minimal training.
Dustless, Clean Installation
Minimal on-site construction and fabrication.
Easy to Clean
Smooth, uniform wall surfaces allow for easy disinfection.
Easy to Configure
Modular components allow for unlimited design potential.
Versatile
Easily expand, relocate or reuse to adjust to changes in demand.
Class “A” Material
Tested in accordance with ASTM E-84 requirements for flame spread and smoke density.
PE Stamped Drawings
Sound Deadening
Also Check: Fluconazole 150 For Yeast Infection
Understanding The Ashrae 170 Requirements For Airborne Infectious Isolation Rooms
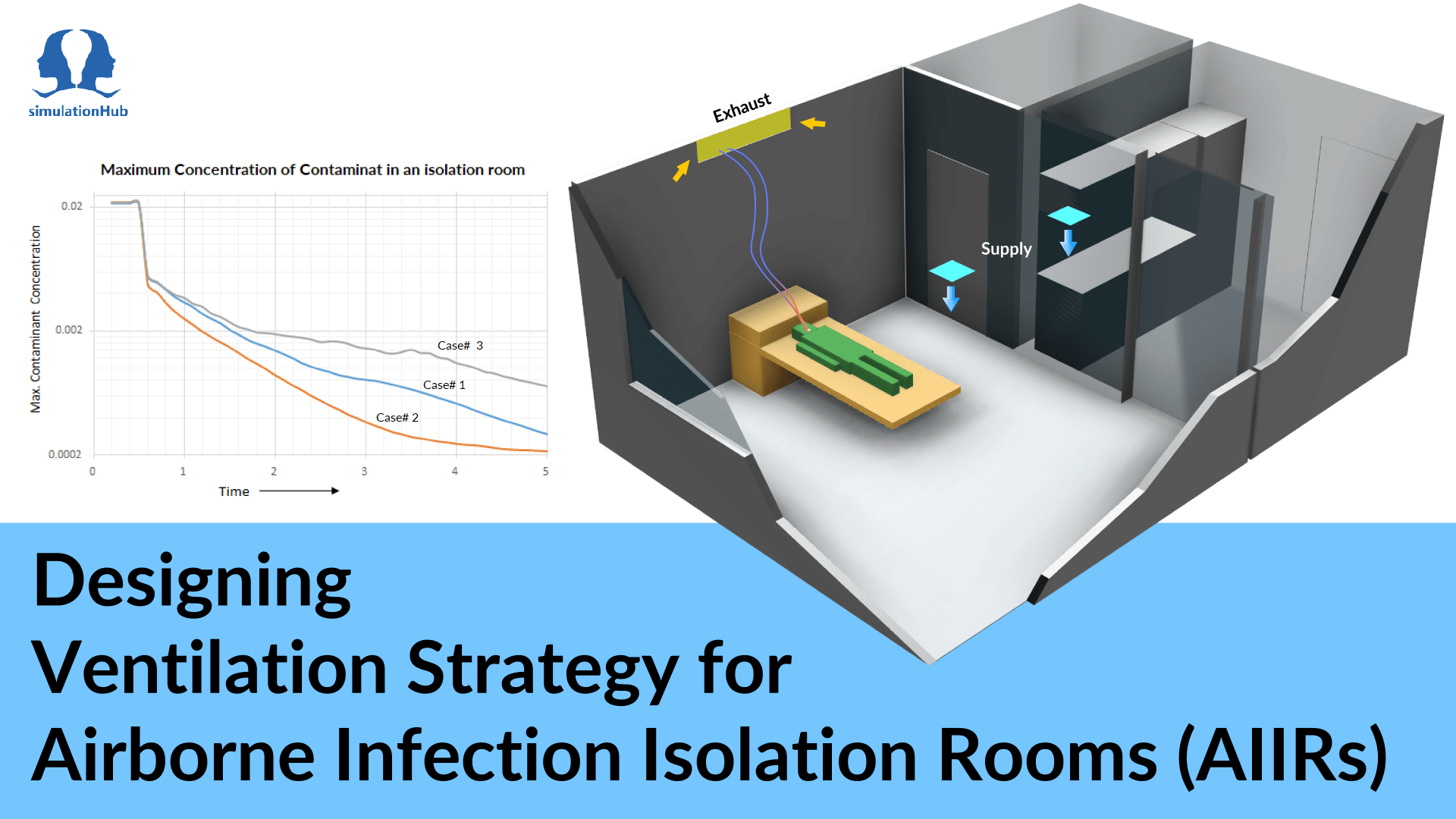
An airborne infectious isolation room, or AIIR, is a type of isolation room that isolates patients infected with organisms that can spread via small airborne droplets . The purpose of an AIIR is to prevent the spread of infectious diseases from an infected patient to others. AIIRs are designed according to the requirements of ASHRAE Standard 170: Ventilation of Health Care Facilities.
| The Antec Controls Touchscreen Room Pressure Monitor , seen here mounted outside each AIIR, provides visible and audible alarms if room pressure is lost |
What Is An Anteroom
This is relatively clean and frequently used area to transition patients/healthcare workers in and out of the airborne isolation room when it is under negative pressure. An anteroom is frequently used as a transitional space between the airborne isolation room and the hallway. It is in this transition area where healthcare workers store their PPE and put on their PPE before entering the airborne isolation room. Ideally, an instrument or monitoring device will display differential pressure values between the anteroom and the Airborne Isolation Room as well as between the anteroom and the hallway.
Recommended Reading: When To See A Doctor For Yeast Infection
What Are Hospital Isolation Rooms
In hospitals and other healthcare facilities, controlling the spread of infectious diseases is critical to keeping patients, personnel, and visitors safe and healthy. An important element of a comprehensive infection control strategy is the use of isolation rooms. These specialized rooms are designed to decrease the likelihood of cross-infection among people within the facility by controlling the flow of air within the room to reduce airborne infectious particle levels. They can achieve this goal in a number of ways, including by controlling the quantity and quality of intake or exhaust air, maintaining an air pressure differential between adjoining areas, directing airflow in a specific pattern, diluting room air with large volumes of clean air, and cleaning the air with high-efficiency particulate air filters.
American Institute Of Architects
A professional organization that develops standards for building ventilation, The 2001Guidelines for Design and Construction of Hospital and Health Care Facilities, the development of which was supported by the AIA, Academy of Architecture for Health, Facilities Guideline Institute, with assistance from the U.S. Department of Health and Human Services and the National Institutes of Health, is the primary source of guidance for creating airborne infection isolation rooms and protective environments
Don’t Miss: How Do Doctors Check For Sinus Infection
Infection Control And Prevention Program
A multidisciplinary program that includes a group of activities to ensure that recommended practices for the prevention of healthcare-associated infections are implemented and followed by HCWs, making the healthcare setting safe from infection for patients and healthcare personnel. The Joint Commission on Accreditation of Healthcare Organizations requires the following five components of an infection control program for accreditation:
The infection control program staff has the ultimate authority to determine infection control policies for a healthcare organization with the approval of the organizations governing body.
Types Of Hospital Isolation Rooms
Isolation facilities can be configured in several ways, including the following:
- Standard Rooms. These rooms utilize standard room air pressure levels. They have normal HVAC systems and may or may not have a clinical handwash sink, en suite shower and toilet facilities, and a self-closing door. While they are generally used for patient contact isolation applications, they can be used for normal patient care when isolation is not required.
- Airborne Infection Isolation Rooms. These roomsalso referred to as infectious isolation roomsutilize a negative-pressure differential. They have lower pressure levels than adjacent rooms so air will rush inward rather than outward when the room is opened. This design prevents airborne infectious particles from escaping into other areas of the healthcare facility. They are employed as single-occupancy rooms to isolate patients with suspected or confirmed airborne-transmissible infections.
- Protective Environment Rooms. These rooms utilize a positive-pressure differential. They have higher pressure levels than adjacent rooms so air will rush outward rather than inward when the room is opened. This design prevents airborne infectious particles from entering the room from other areas of the facility. They are utilized to protect immune-compromised patients from airborne-transmissible infections.
Recommended Reading: How To Avoid A Yeast Infection While Taking Antibiotics
Guidance On Anteroom Use
There is a lack of consistency in construction guidance for AIIR anterooms across various professional organizations and federal agencies. Table 1summarizes the recommendations by various US and international agencies and organizations on isolation anteroom requirements.15, 16, 17, 18, 19, 20 Negative pressure isolation rooms in both the United Kingdom and some states of Australia are required to have anterooms between patient AIIRs and adjacent corridors, but in the United States they are not required. A recent recommendation in the UK incorporates a modified design of an isolation room called a Positive Pressure Ventilated Lobby room.12 If anterooms are included in the design, US guidelines, similar to Australian guidelines, call for isolation rooms to be maintained at a negative pressure compared with the anteroom and, in turn, the anteroom to be maintained at a net negative pressure compared with the corridor.
The Typical Challenges In An Isolation Situation
How can one prevent microbes from spreading in the hospitals isolation ward, and how are patients best protected when they have reduced immune capabilities? How to avoid the costly situation of empty isolation rooms in normal conditions yet utilise the rooms well when there is a need for isolation? Halton has the answers.
Do you have a challenge that requires a solution?
Consult us. Lets see whether we have a ready-made solution for you or can create one together.
Don’t Miss: I Ve Had A Sinus Infection For 2 Months
What Are Airborne Infection Isolation Rooms
Airborne Infection Isolation rooms, commonly called negative pressure rooms, are single-occupancy patient care spaces designed to isolate airborne pathogens to a safe containment area. AII rooms are a specialized application of a hospitals HVAC system, where the airflow supplied into the room is balanced with exhaust airflow to create at least -0.01 WC negative differential pressure with respect to an adjacent space, usually the hallway or an anteroom. In simple terms, this provides a gentle flow of air under a closed doorway and into the room so that no airborne particulates escape into nursing staff or public areas. Exhaust from these rooms is not recirculated in the HVAC system. Instead, exhaust air typically moves in dedicated ductwork to ventilation stacks on the rooftop, where atmospheric air provides sufficient dilution to make the resulting air safe.
The use of AII rooms is required by the Centers for Disease Control and Prevention as a means to protect the public from the spread of disease. Patients immediately confined to AII rooms usually have illnesses such as tuberculosis, SARS, H5N1, or coughing conditions that may pose a risk to hospital staff. In response to the CDCs AII room mandate, the American Society of Heating, Refrigerating, and Air-Conditioning Engineers outlines how airflow should be designed in these spaces. ASHRAE Standard 170 specifies air change rates, pressure requirements, temperature guidance, and filtration conditions.
Instructions For Establishing Expedient Patient Isolation Room For Surge Airborne Isolation Capacity Within A Traditional Healthcare Environment
Background
Although they could be modified to conform to an alternate care site, the following instructions describe the creation of expedient airborne infection isolation within a traditional healthcare patient room. The expedient isolation techniques described are intended to be an emergency alternative to establish surge capacity in airborne infection isolation. It is intended for use during an infectious disease emergency when insufficient engineered airborne infection isolation rooms are available to meet patient demand. Selection of patient areas suitable for conversion into expedient patient isolation room configurations should be made in consultation with the healthcare facilitys safety officer, infection control, and building facilities department participation. Selected patient isolation zones should be evaluated to ensure fire sprinkler coverage is not significantly impaired by the isolation curtains. The inner patient isolation zones should not include recirculating HVAC wall units or HVAC return air grills unless they can be sealed shut or otherwise isolated from the inner isolation zone. Depending upon the patient room, the zone-within-zone configuration may be set up to serve one or two patients. The following instructions are for the two-patient scenario. The single-patient scenario may be established following the same directions, but with the HEPA filtration systems inlet rotated ninety degrees such that it serves just the one inner isolation zone.
Don’t Miss: Natural Antibiotic For Ear Infection In Adults
Lewis J Radonovich Jr
aNational Center for Occupational Health and Infection Control, North Florida/South Georgia Veterans Health System, Gainesville, FL
dDepartment of Medicine, University of Florida, Gainesville, FL
Despite their importance, guidance on the construction of anterooms is less than clear. We provide arguments in support of building anterooms alongside AIIRs. We also review the guidance by various organizations on this topic and urge that the guidelines be made firmer in support of the construction of anterooms for AIIRs.