Surgical Mesh Can Be Dangerous Inside The Body
It does not take too much of a stretch of the imagination to understand how surgical meshes made from the same material as the things listed above can cause side effects when it is implanted inside the body.
While surgical meshes are effective in the majority of patients who have hernia repair surgeries, there is a high rate of complications. Nearly 4% of patients who have hernia mesh surgery will experience hernia mesh complications.
When a person has hernia mesh complications, they can be serious and long-lasting. It is not uncommon for a patient to never be the same again after hernia repair surgery.
Late Ps Aeruginosa Inguinal Mesh Infection 12 Years After The Initial Operation: Report Of The Case And Short Review Of The Literature
Dimitrios Filippou
1Department of Laparoscopic Surgery and Surgical Oncology, Neo Athinaion Hospital, Athens, Greece
2Department of Anatomy and Surgical Anatomy, Medical School, University of Athens, Athens, Greece
Abstract
Inguinal hernia mesh repair is one of the most frequent operations performed worldwide. The Lichtenstein technique and its various modifications are the most popular operations for groin hernia repair. The rate of surgical site infection following inguinal hernia repair ranges between 0 and 14% in various series. Most of these infections developed early postoperatively. The incidence of late mesh infection following open inguinal hernia repair still remains unclear and highly variable. Late deep mesh infections are relatively rare specially after more than 10 years. The most common pathogens reported in the literature are E. coli and St. aureus. The infection is treated by conservative means initially but in case of failure then the mesh should be removed surgically. A unique case of a patient with very late mesh infection is presented. The infection was due to Pseudomonas aeruginosa, which occurred 14 years after the initial operation and presented as subcutaneous fistula.
1. Introduction
Lichtenstein technique is an open surgical technique for inguinal hernia repair based in the enhancement of the weakened inguinal floor by tension-free placing of a polypropylene mesh .
2. Report of the Case
Ps. aeruginosa
3. Discussion
Data Access
Controllable Risk Factors For Ssi
The implementation of evidence-based protocols to prevent SSIs can substantially decrease the incidence of SSIs and healthcare costs after abdominal hernia surgery. These include CDC, NICE and WHO guidelines for the prevention of SSIs, Enhanced Recovery After Surgery protocols and Perioperative Quality Initiatives.13,33,50,51
These are based on systematic reviews and consensus statements and relate to:
Control of contaminated airborne particles in the operating theatre .
Patient selection and preparation .
Surgical technique/heuristics .
Implementation of evidence-based guidelines includes patient selection for elective hernia repair, pre-operative risk interventions, improved operative technique and centralization of complex hernia surgery. This is related to modifiable comorbidities which increase the incidence of SSI, including tobacco smoking, obesity and diabetes mellitus. A quality improvement initiative at a single-centre safety-net US academic institution included establishment of a complex hernia specialist unit and the implementation of 6 evidence-based interventions:
Mesh reinforcement is recommended for elective VHR with no contamination.
Laparoscopic repair is recommended for clean elective VHR.
Read Also: Best Abx For Ear Infection
Removal Of The Infected Mesh Alone
In the following two studies, a total of 47 patients with mesh infection were treated by means of partial or complete mesh removal. Neither a synthetic nor a biological mesh was implanted to replace the explanted mesh.
In a retrospective case series by Akyol et al., 15 mesh removals were performed after inguinal hernia repair because of chronic mesh infection in 14 males and 1 female with a median age of 52 years . At the time of presentation, 13 patients had chronic sinus at explanation, while 2 had abscesses. The interval from hernia repair to mesh removal was 4204 months. The infected meshes were completely removed. None of the patients had the transversalis fascia reinforced, due to thickening by fibrosis from the former mesh. Follow-up was performed median 62 months . Infection resolved successfully in all patients. One patient reported paresthesia and another developed a recurrent hernia.
In a retrospective case series by Tolino et al., 32 mesh removals were performed due to chronic infection, 22 after incisional and 10 after inguinal hernia repair . The interval from repair to mesh removal ranged from 4 to 60 months. A total of 51 operations in the 32 patients were needed for definitive treatment, including partial or total mesh removal. The average follow-up was 40 months . Five hernia recurrences and one intestinal fistula were observed after incisional mesh removal. One recurrence and one fistula developed after inguinal hernia mesh removal.
Absorbable Vs Permanent Mesh

A synchronous hernia mesh repair should not be contraindicated during other intra-abdominal operations .8,9,11 An extraperitoneal mesh repair rather than intraperitoneal mesh repair is preferable in contaminated VHR, emergency VHR, emergency laparotomy or with concurrent colorectal surgery.9,11,40,41 Some surgical societies including the WSES and the Ventral Hernia Working Group advocate the use of simple suture or biological mesh in contaminated/dirty VHR cases. However, this approach has not been shown to be superior to macroporous polypropylene VHR with respect to SSI, surgical site occurrence , unplanned re-operation, cost or hernia recurrence in recent systematic reviews11,37,40,41 . This is important when resources are limited, as the cost of a single biological mesh can be equivalent to 100 permanent synthetic meshes.37
Fig. 3
Forest plot comparing odds ratio of SSI after VHR using non-absorbable synthetic mesh or absorbable mesh in a contaminated field. Overall, the use of absorbable mesh was associated with a 2.84 increased OR of SSI. Reproduced by permission41
Recommended Reading: Can You Get Antibiotics For A Sinus Infection
The Studies Were Published Between 2007 And 2020
Six studies with 4092 patients compared mesh and suture repairs.
Five studies analyzed mesh repair in patients by field contamination level with a total of 34161 patients.
Four studies comprising 1148 patients reported SSI, comparing mesh repair technique with synthetic mesh or other type of meshes.
Hernia Surgeries Are Big Businesses For Hospitals
There are over one million of hernia repair procedures in the United States each year. Most of these are for hernias in the groin, but around 20% of these surgeries are for procedures in the abdominal cavity.
The total expenditure on hernia repair surgeries can top $48 billion. The most common type of procedure is laparoscopic inguinal hernia repair. The patient is in and out of the hospital in the same day, and the total procedure is completed in less than 45 minutes.
These are very profitable procedures for hospitals and doctors. The average hernia procedure runs around $8,000, depending on the hospital and market.
Doctors and hospitals have every incentive to perform hernia mesh repair as quickly as possible, so they can keep billing insurance and making money.
Quicker surgical procedures have high profit margins, and doctors may recommend this operation without considering the full range of risk factors in the patient and the possibility of mesh complications.
Hernia meshes are also very profitable for the companies that make them. Ten years ago, this little piece of plastic, that does not cost that much to make, cost patients nearly $36. With inflation, that price has increased.
You can imagine how the profit margins in making hernia mesh are very high.
Don’t Miss: Chances Of Getting Hiv From Infected Needle
Systematic Review And Meta
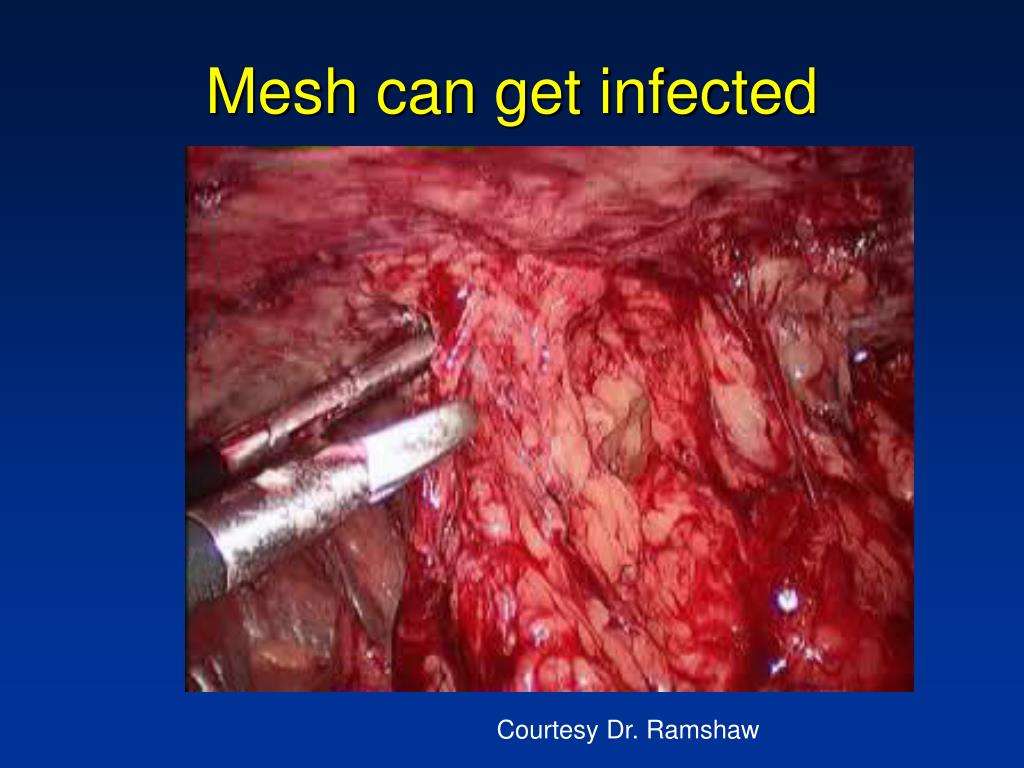
Surgical mesh infection is a devastating complication in hernia repair.
-
The main risk factors for SMI are open and emergency surgery, and onlay position.
-
Other identified risk factors are prolonged surgery, obesity, steroids use, ASA status and diabetes.
-
The identification of high-risk patients may contribute to mitigation of SMI impact.
Evidence For Replacement Of An Infected Synthetic By A Biological Mesh In Abdominal Wall Hernia Repair
- 1Department of Surgery, Skane University Hospital, Malmö, Sweden
- 2Department of Surgery, Asklepios Hospital Harburg, Hamburg, Germany
- 3Department of Surgery, Centre for Minimally Invasive Surgery, Vivantes Hospital Berlin, Academic Teaching Hospital of Charité Medical School, Berlin, Germany
Introduction: The incidence of deep infection using a synthetic mesh in inguinal hernia repair is low and reported to be well below 1%. This is in contrast to incisional hernia surgery where the reported incidence is 3% respective 13% comparing laparoscopic to open mesh repair reported in a Cochrane review. Main risk factors were long operation time, surgical site contamination, and early wound complications. An infected mesh can be preserved using conservative treatment were negative pressure wound therapy could play an important role. If strategy fails, the mesh needs to be removed. This review aims to look at evidence for situations were a biological mesh would work as a replacement of a removed infected synthetic mesh.
Materials and methods: A literature search of the Medline database was performed using the PubMed search engine. Twenty publications were found relevant for this review.
Recommended Reading: Amoxicillin Vs Penicillin For Tooth Infection
Replacement Of The Infected With A Biological Mesh
In the following six studies , a total of 92 patients with mesh infection were treated by mesh removal followed by implant of a biological mesh in ventral hernia patients.
In a retrospective case series, Albino et al. reported on 27 patients with an infected synthetic mesh treated with a multi-staged approach . The initial surgical procedure consisted of abdominal exploration with debridement and mesh removal followed by VAC® therapy. In the second stage, all patients underwent component separation and hernia repair reinforced by porcine acellular dermal matrix . Primary fascial closure was achieved in 21 of patients . Bridging was performed in six patients. The average follow-up was 32 months . Six patients were found to have wound dehiscence and five of these had had clinical evidence of a surgical site infection. Wound healing was achieved in all patients in average after 8 weeks . Five patients developed a recurrent hernia. Both bridging and a postoperative infection were found to increase the risk of a hernia recurrence .
Two patients were presented in a case report by Cavallaro et al. where one preperitoneal Prolene® mesh and one retromuscular polypropylene mesh were extracted and replaced with a retromuscular bovine pericardium graft. No complication and no recurrences were reported after 5 and 4 years, respectively. Closure of the gap was not reported on .
Which Mesh Should Surgeons Use
When choosing a mesh , the surgeon must consider the context in which it is to be used. In most situations, one should look for a light-weight mesh, with large pores and minimal surface area. Ideally, it should consist of a monofilament. A polypropylene or polyester mesh is, therefore, usually suitable . These meshes will be more comfortable and have a lower risk of infection. If the mesh is to be placed inside the peritoneal cavity, an attempt should be made to minimise adhesions by choosing a hybrid mesh with an absorbable surface. Despite manufacturers’ claims, the differences between the various types of these are unproven and it is currently difficult to recommend a single material. In infected wounds, an absorbable mesh is preferred, for example, polyglactin or polyglycolic . Biomaterials may also be useful in this situation if the additional cost can be justified. Finally, the surgeon should not forget that the way the mesh is placed is as important as the type of mesh used. If a mesh is too small or fixed under tension, there will be complications whatever its material. Despite the new implants available, surgical skill still has a role in preventing hernia recurrence!
Also Check: Does Kidney Infection Go Away By Itself
Data Sources And Search Strategy
An extensive electronic search of the relevant literature was performed by the authors on 31 December 2020. The Keywords used for the final search using the following databases: MEDLINE, the Cochrane Library, Scopus, Embase were strangulated,incarcerated,acute,complicated,contaminated,mesh,prosthesis,ventral hernia,incisional hernia, abdominal wall hernia and surgical site infection. Additionally, references from eligible articles and reviews on the topic not found in the literature search were reviewed. No language restrictions were applied.
Are There Any Mesh Products More Prone To Infection

Physiomesh and Atrium C-QUR mesh are the subjects of lawsuits specifically due to mesh-related infections. They use polypropylene mesh, a problematic synthetic mesh.
Extended polytetrafluoroethylene and polyethylene terephthalate are also prone to infection. And mesh with small pores tend to trap bacteria more than mesh with large pores. The safest pore size is 75 micrometers.
Hernia patients should speak with their surgeons about alternatives to synthetic meshes, such as biologic meshes. 6
Don’t Miss: Best Antibiotic For Severe Sinus Infection
How Is Infection Diagnosed And Treated
Radiological imaging can help your physician determine if the mesh is indeed infected. Examples include ultrasounds and CT scans.
Once the patient is diagnosed with an infection, medical and surgical treatment may be necessary. The combination of the two would include antibiotics, intravenous antimicrobial agents, and/or surgery for mesh removal.
A study concluded that 63% of patients with mesh-related infections are infected with MRSA .5 Unlike staphylococcal bacteria, MRSA is extremely difficult to treat.
In addition, antibiotics may not even be able to reach the infected area since bacteria creates a biofilm capsule around the mesh. This is why surgery is often required to treat infections.
Complications Related To Hernia Meshes
Even a repaired hernia can continue to present danger to the patient when there is a polypropylene mesh still inside the body. The human body does not always take well to a foreign substance inside it, especially one that is chemical and not biological.
In addition, the body is relying on the integrity of a synthetic substance. If the plastic breaks down over time , it can cause other serious side effects inside the body.
Read Also: Get Yeast Infection Prescription Online
Should I Contact A Personal Injury Lawyer
Yes. People who suffered an incidence of infection from their hernia mesh or revision surgery may be entitled to large financial compensation from the manufacturer and/or their surgeon.
Currently there are federal multi-district litigations against Ethicon in Georgia, Bard Davol in Ohio, and Atrium in New Hampshire amounting to more than 18,000 plaintiffs. And thousands of victims are bringing individual lawsuits against Covidien and Gore.
Our lawyers at Shouse Law Group create attorney-client relationships throughout the United States with victims who have suffered injuries from defective mesh products. Call our law firm today for a free consultation. We take no money unless we win your case.
References
Symptoms Of Hernia Mesh Complications Or Failure
Many patients will come home from the hospital or surgical center after their incisional hernia repair, and they will be feeling fine. However, hernia mesh can be a ticking time bomb in the body of some patients.
They may not even begin to feel mesh complications until months or years after their surgery.
Hernia mesh is a synthetic medical device and mesh failure often happens over time instead of right after the surgery. There is no exact timetable about when patients may begin to feel mesh complications from inguinal hernias. It could be a few weeks or a few years.
Also Check: Ear Infection Treatment Adults Over The Counter
Replacement Of The Infected With A New Synthetic Mesh
In a single surgeon case series by Birolini et al., a 16-year retrospective review based on a prospective protocol was carried out in 41 patients having had ventral hernias surgery with their meshes removed . A total of 27 patients had a supportive infection and 14 had an exposed mesh. Bowel resection or an associated contaminated procedure was performed in 15 patients. An onlay polypropylene mesh was used for replacement in all patients. In the short-term follow-up, all, except one mesh, could be preserved. Three recurrences were seen after a mean follow-up of 74 months, out of which one was associated with an intestinal fistula. A total of 95% of the patients were considered cured from their chronic mesh infection. It was concluded that onlay polypropylene mesh yielded favorable outcomes, for high-risk ventral hernia patients, having an infected synthetic mesh removed in a single-stage repair setting.
Introduction: Mesh And Hernia Repair
The clinical use of Marlex polyethylene mesh in 1959 for incisional ventral hernia repair and then Marlex knitted polypropylene mesh for inguinal hernia repair ushered in a new paradigm in the repair of abdominal wall herniae.1,2 The Lichtenstein mesh repair for inguinal hernia and modified Stoppa-Rives preperitoneal and retro-rectus mesh repairs subsequently became the standard in hernia surgery. Mesh reinforcement allowed tension-free repairs, improved perioperative pain and shortened hospital stay, and was associated with decreased long-term hernia recurrence rates.3 For example, in a 2014 pooled analysis of 637 sutured versus 1145 synthetic mesh repairs of primary ventral hernia, the respective recurrence rate was 8.2% vs 2.7% .4 A 2016 meta-analysis of randomized controlled trials of sutured versus mesh repair of incisional and primary ventral hernia found a significant reduction in hernia recurrence with the use of mesh â=â0.36 95% CI, 0.27 to 0.49 p< â0.00001).5 The risk of re-operation for recurrence after Lichtenstein repair was 25% of that of sutured repair in an analysis of the Danish Hernia Database involving 47,975 male patients 5 years or more after primary IHR â=â0.25 . Sutured repairs in this series included McVay, Shouldice, annulorrhaphy or Bassini repair .6
Fig. 1
Read Also: Can A Yeast Infection Be A Sign Of Pregnancy
Patient Characteristics And Clinical Outcomes
A total of 75 patients reporting VHWG grade II or III who underwent primary ventral hernia or incisional hernia repair with a follow-up of at least 18 months were included in the Italian Hernia Club registry on 13th June 2019. Table reports the patients characteristics.
Table 1 Summary of patient demographics and comorbid conditions.
The Difficulties Of Hernia Mesh Removal
Hernia mesh can be difficult to remove from the body, even when it does not disintegrate or migrate. The mesh can become intertwined with the muscle.
Alternatively, hernia mesh could adhere to internal organs, and it could be difficult to take the mesh out without damaging the organ. You cannot always assume that the doctor can easily reverse a hernia mesh procedure by easily removing surgical mesh devices.
This could also require several surgeries, or it may not even be completely possible.
Don’t Miss: How To Get Antibiotics For Tooth Infection