Disseminated Infection With Mycobacterium Avium Complex
Patients who have been treated for disseminated Mycobacterium avium complex disease should continue to receive full therapeutic dosages of antimycobacterial agents for life .8 Unless good clinical or laboratory evidence of macrolide resistance exists, the use of a macrolide antibiotic is recommended in combination with ethambutol with or without rifabutin .9,10 Treatment of MAC disease with clarithromycin in a dosage of 1,000 mg twice a day is associated with a higher mortality rate than has been observed with clarithromycin administered at 500 mg twice a day thus, the higher dosage should not be used .11,12 Clofazimine has been associated with an adverse clinical outcome in the treatment of MAC disease and should not be used .12,13
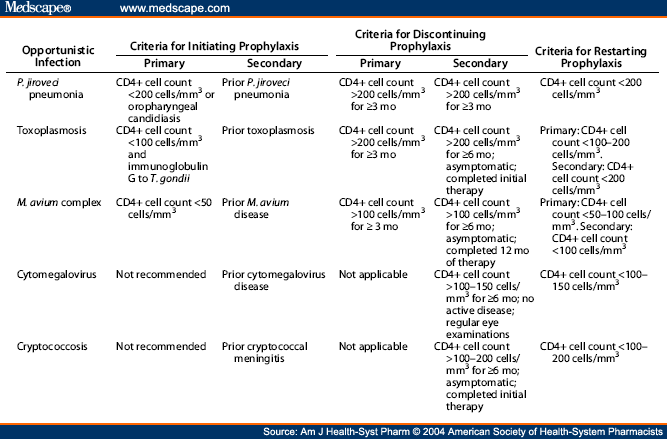
Discontinuation of Secondary Prophylaxis . Although patients receiving chronic maintenance therapy for MAC might be at low risk for recurrence of MAC when their CD4+ T-lymphocyte counts increase to greater than 100 per mm3 following six to 12 months of HAART, the number of patients who have been evaluated is insufficient to warrant a recommendation to discontinue maintenance therapy in such patients.
Drug Interactions. Rifabutin should not be administered with certain protease inhibitors or nonnucleoside reverse transcriptase inhibitors . Although protease inhibitors might also increase clarithromycin levels, no recommendation to adjust the dosage of clarithromycin or protease inhibitors can be made on the basis of existing data.
Primary And Secondary Prophylaxis Against Opportunistic Infections In Hiv Aids
|
TMP-SMX SS or DS daily |
TMP-SMX DS 3x weekly Dapsone 100mg daily or 50mg BID* Atovaquone 1500mg daily |
||
|
Toxo IgG + and CD4 < 100** |
TMP-SMX DS daily |
TMP-SMX SS daily or DS 3x weekly Dapsone 50mg daily * + pyrimethamine 75mg qweek + leucovorin 25mg qweek Atovaquone 1500mg daily +/- pyrimethamine 25mg daily +/- leucovorin 10mg daily |
|
|
Mycobacterium avium complex |
|
Azithromycin 1200mg q week |
Azithromycin 600mg 2x weekly |
*Rule out G6PD deficiency prior to initiating dapsone therapy
** If on PCP prophylaxis not active against toxo , retest toxo serology if CD4 falls < 100 for initiation of appropriate prophylaxis
Initial Tests And Prophylactic Regimens
On the patient’s first visit, serologies for syphilis hepatitis A, B, and C and toxoplasmosis should be obtained. Although the incidence of CMV disease, including retinopathy, has declined significantly, it is recommended that patients with HIV who are not at high risk for CMV infection be screened to confirm that they are CMV-negative . Such HIV-positive, CMV-negative persons would be instructed to limit exposure to CMV by using latex condoms and other barrier precautions , be informed of the risk for acquisition in daycare facilities , and be instructed to accept only CMV-seronegative or leukocyte-reduced blood products in nonemergent situations .
Also Check: How To Alleviate Bladder Infection Pain
Appendix : Pico Questions
- 2 What is the epidemiology of candidiasis in individuals living with HIV?
- 2.1 What are the main Candida spp. causing Candida infections in recent surveys of people living with HIV?
- 2.2 What are the main risk factors for Candida infection in people living with HIV?
- 3.1 What are the clinical manifestations of mucosal candidiasis in people living with HIV?
- 4.1 When is it appropriate to request microbiological confirmation of Candida infections?
- 4.2 What are the preferred techniques for microbiological diagnosis of Candida spp.?
- 4.3 When should endoscopy be used to diagnose suspected oesophageal candidiasis?
- 5.1a What are the preferred treatments for oropharyngeal candidiasis?
- 5.1b What is the role of topical therapy?
- 5.2. What are the preferred treatments for oesophageal candidiasis?
- 5.3 How should fluconazole-refractory candidiasis be treated?
- 5.4 What are the preferred treatments for vulvovaginal candidiasis?
- 5.5 How should invasive candidiasis be treated in people living with HIV?
- 6.1 Is prophylaxis to prevent mucosal candidiasis recommended for people with advanced HIV infection?
- 6.2 Is continuous azole therapy recommended?
Are Opportunistic Infections Common In People With Hiv
Before HIV medicines were available to treat HIV infection, opportunistic infections were the main cause of illness and death in people with HIV. HIV medicines are now widely used in the United States so fewer people with HIV get opportunistic infections. By preventing HIV from damaging the immune system, HIV medicines reduce the risk of opportunistic infections.
However, opportunistic infections are still a problem for many people with HIV. Some people with HIV get opportunistic infections for the following reasons:
- About 15% of people who have HIV dont know that they are infected. An opportunistic infection may be the first sign that they have HIV.
- Some people who know they have HIV arent getting treatment with HIV medicines. Without HIV treatment, they are more likely to get an opportunistic infection.
- Some people may be taking HIV medicines, but the medicines arent controlling their HIV. Poorly controlled HIV can be due to many factors, including lack of health care, poor medication adherence, or incomplete absorption of HIV medicines. People with poorly controlled HIV have an increased risk of getting an opportunistic infection.
Don’t Miss: Is Bactrim Good For Tooth Infection
Enhancing Healthcare Team Outcomes
HIV patients who are untreated are prone to multiple opportunistic infections due to the progressive lowering of their CD4 + T cells. Because of the high morbidity and mortality of these infections, every attempt should be made that these patients have enough resources for early diagnosis of HIV, timely initiation of ART, regular follow up to ensure medication adherence.
These patients should be managed by an interprofessional team that includes an infectious disease specialist, internist, specialist nurse, pharmacists, and social workers. They also need close monitoring with regular lab work to evaluate for improvement of CD4+ cell count, assessment of medication-related side effects, and the emergence of opportunistic infections. Patients with HIV often face social stigma due to their infections. The team must additionally ensure adequate social and financial support, rehabilitation for intravenous drug abusers along with patient education regarding safe sex practices, and avoidance of high-risk behaviors.
Primary Prophylaxis As The Standard Of Care
P jiroveci pneumonia
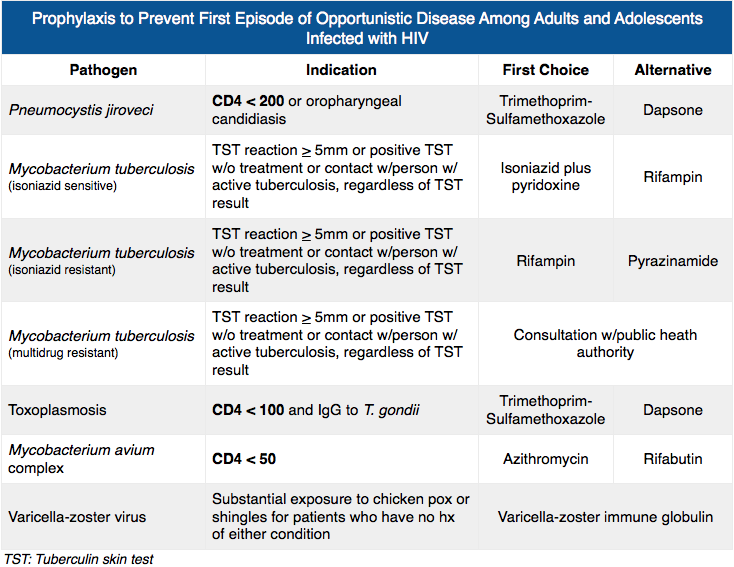
Indications for PCP prophylaxis include a CD4 count of fewer than 200 cells/L or less than 14% of lymphocytes . The preferred regimen is trimethoprim-sulfamethoxazole 1 double-strength tablet orally daily or 1 double-strength tablet orally 3 times weekly. Alternatives include dapsone 100 mg orally daily , aerosolized pentamidine 300 mg administered via the Respirgard II nebulizer monthly , or atovaquone suspension 750 mg orally twice daily).
Latent Mycobacterium tuberculosis infection and exposure
Tuberculosis is both the leading cause of death from infectious disease globally and the leading cause of morbidity and mortality among people living with HIV. Screening for TB in the HIV-infected population has been suboptimal, with only 47% to 65% of patients completing screening. The most common predisposition for TB is birth or residence outside of the United States. All persons with HIV should be tested for LTBI regardless of their epidemiologic risk for TB exposure . All newly-diagnosed patients with HIV infection should be screened with a tuberculin skin test or interferon-gamma release assay , and re-screened once the CD4 count rises to 200 if initially less.
Active TB should be excluded by lack of symptoms and negative chest radiograph before prophylactic regimens are started. Active TB may be more likely in a patient with previous active TB than in a patient without a history of TB.
M avium complex infection
Toxoplasma gondii infection
Syphilis
You May Like: Are There Different Types Of Uti Infections
Drugs To Prevent Opportunistic Infections
Certain antibiotic medicines can be used to prevent some common opportunistic infections in people with HIV/AIDS.
However, your doctor will consider the risks and benefits of antibiotics for preventing infection in your situation. Antibiotics can lead to drug resistance, and they can disrupt the balance of the microbes in your gut, which can increase your risk for certain gastrointestinal infections.
Antibiotics to prevent tuberculosis . Latent TB infections are common and dangerous to someone diagnosed with HIV. As CD4 counts drop, a latent TB infection can reactivate.
A latent TB infection is diagnosed by a tuberculin skin test or by a blood test. Doctors often combine isoniazid and rifamycin antibiotics in a âdrug cocktailâ to prevent latent TB from turning into active TB. Your doctor may also start this treatment if you have been exposed to someone with active TB, even if you donât test positive for latent TB.
Rifamycin antibiotics can interfere with ART. If youâre already on ART and are diagnosed with latent or active TB, your doctor may either change your ART drugs or use an alternative drug to treat your TB. Your doctor may need to tweak your regimen to make sure both treatments are working safely and effectively and monitor you to keep an eye on any toxic side effects. Rifamycin antibiotics can also lead to drug resistance fairly quickly, so you usually take them in combination with other drugs.
Antibiotic drugs used to prevent MAC disease include:
Strategies To Prevent Mucosal Candidiasis In Patients With Advanced Hiv Infection
Routine prophylaxis is not warranted and is associated with the emergence of resistance. As with other opportunistic infections, effective cART prevents relapses of symptomatic oropharyngeal or oesophageal candidiasis. Thus, the most successful strategy for managing patients with candidiasis is to commence cART , . Drugdrug interactions should be considered with regard to antiretroviral and antifungal agents . Systematic review and meta-analysis of the impact of cART on opportunistic infections in low- and middle-income countries confirms that cART dramatically reduces the incidence of mucosal candidiasis with oral candidiasis being one of the opportunistic infections with the greatest impact . A casecontrol study in a high-income setting examining the risk of oesophageal candidiasis showed that cART is associated with a reduced odds ratio of oesophageal candidiasis . There are rare reports of candidiasis associated with immune reconstitution inflammatory syndrome, including a case of Candida meningitis leading to fatal vasculitis . Despite the dramatic decline in candidiasis with cART, there remains a residual level in people living with HIV above that in HIV-seronegative individuals , .
Don’t Miss: How To Take Care Of A Tooth Infection
Role Of Microbiological Confirmation Of Candida Spp Infection
Oropharyngeal and oesophageal candidiasis are clinical diagnoses, and microbiological confirmation has traditionally not been advised due to the likelihood of positive cultures in the absence of clinical disease. Recent studies highlight that, even in the era of widespread antiretroviral therapy, non-oral health specialists can accurately identify oropharyngeal candidiasis with 8190% sensitivity and 92% specificity, which approaches the performance of microbiological detection . This suggests that this approach is still reasonable for mucosal infections caused by Candida spp. There is increasing recognition that empiric antimicrobials and low-dose prophylaxis in settings of minimal risk promote resistance in fungi .
Candida cultures should be requested for individuals with persisting signs and symptoms of infection despite antifungal therapy or who experience recurrent infection. This will serve to identify the possibility of an azole-resistant infection or, in the context of negative cultures/poor response despite susceptible strains, will indicate the possibility of alternative or additional diagnoses. Recurrent oropharyngeal candidiasis occurs in the context of failure to establish immune reconstitution or the presence of persistent non-HIV-related risk factors and has represented a primary driver for the selection of non-albicans Candida and of fluconazole-resistant species due to repeated antifungal exposure , , , .
Fungal Or Yeast Infections
According to current NIH guidelines, Cryptococcus neoformans and Candida infections do not warrant primary prophylaxis. In the case of Cryptococcus infection, primary prophylaxis has not been shown effective in Thailand. New WHO guidelines recommend cryptococcal antigen testing and preemptive therapy in antigen-positive patients with a CD4 count < 100 cells/uL in Africa and other areas of high prevalence. Prolonged suppressive therapy for Candida is not recommended owing to risk of resistance. However, if necessary because of frequent recurrence or severe disease, fluconazole 100 mg PO thrice weekly for thrush , fluconazole 100-200 mg daily , or fluconazole 150 mg PO once weekly are the first recommended drugs.
Fortunately, aspergillosis and phycomycosis are rare in individuals infected with HIV. These infections should be considered in patients with invasive sinusitis and focal pulmonary lesions but do not warrant prophylaxis.
Travelers to malaria-prone areas should have malaria prophylaxis, and those who live in such areas should practice preventative measures, such as the use of treated mosquito netting.
You May Like: Natural Tooth Pain Relief Infection
Therapies To Keep Infections From Coming Back
Preventive drugs can be used in two key ways: preventing first-time infections and preventing infections from coming back .
In people with AIDS, serious fungal infections or viral infections often come back, so you may have to take secondary prophylaxis for a long time after an initial infection. This will depend on your CD4 count and the type of infection.
The herpes virus can also come back, so you may take âsuppressive therapyâ long term with an antiviral drug such as acyclovir or valacyclovir after a herpes infection.
Show Sources
Annals of Internal Medicine: âUSPHS/IDSA Guidelines for the Prevention of Opportunistic Infections in Persons Infected with Human Immunodeficiency Virus: A Summary.â
Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine: âBacterial Pneumonia.â
CDC: âGuidelines for Preventing Opportunistic Infections Among HIV-Infected Persons,â âLive Attenuated Influenza Vaccine ,â âToxoplasmosis.â
Cleveland Clinic: âMAC Lung Disease.â
Cogent Medicine: âPrevalence of Bacterial Pneumonia Among HIV-Seropositive Patients in East Africa: Review.â
U.S. Department of Health & Human Services: âFDA-Approved HIV Medicines,â âGuidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV,â âVaccines and People with HIV,â âVaccine Types.â
Johns Hopkins Medicine: âPneumocystis Pneumonia or PCP.â
Mayo Clinic: âVaricella-Zoster Immune Globulin .â
Opportunistic Infection Therapeutic Guidelines
Despite the reduction in the incidence of HIV-related opportunistic infections since the introduction of highly active antiretroviral therapy in 1996, significant numbers of patients continue to present with advanced HIV disease and the full spectrum of opportunistic infections associated with severe CD4 lymphopenia. These infections occur more often in marginalized patient populations who are not engaged in antiretroviral therapy and other preventive measures, such as vaccination programs and opportunistic infection prophylaxis.
Recent changes with respect to opportunistic prophylaxis and treatment include the immune reconstitution inflammatory syndromes , which may occur in approximately 25% of patients who begin HAART in the setting of advanced HIV disease and CD4 counts below 100 cells/mcL. Criteria for discontinuing opportunistic infection prophylaxis have also been established for patients who experienced antiretroviral-therapy-induced immune reconstitution.
Read Also: Can You Take Yeast Infection Medication While On Antibiotics
Why Do People With Hiv Get Opportunistic Infections
Once a person is infected with HIV, the virus begins to multiply and to damage the immune system. A weakened immune system makes it harder for the body to fight off HIV-related opportunistic infections.
HIV medicines prevent HIV from damaging the immune system. But if a person with HIV does not take HIV medicines, HIV infection can gradually destroy the immune system and advance to AIDS. Many opportunistic infections, for example, certain forms of pneumonia and tuberculosis , are considered AIDS-defining conditions. AIDS-defining conditions are infections and cancers that are life-threatening in people with HIV.
Can Opportunistic Infections Be Treated
There are many medicines to treat HIV-related opportunistic infections, including antiviral, antibiotic, and antifungal drugs. The type of medicine used depends on the opportunistic infection.
Once an opportunistic infection is successfully treated, a person may continue to use the same medicine or an additional medicine to prevent the opportunistic infection from reoccurring .
You May Like: Z Pack Good For Sinus Infection
Candida Spp Causing Candida Infections In People Living With Hiv
Candida albicans remains the leading cause of Candida infections globally but the distribution of non-albicans Candida spp. shows geographical variation . Non-albicans Candida spp. occur particularly in association with previous azole therapy and advanced immunosuppression . HIV-specific data for oropharyngeal or vulvovaginal infections reflect the trends in international surveillance data C. albicans remains most prevalent. The rates of non-albicans Candida spp. continue to rise to approximately 30% in many cohorts, influenced by geographical location and resource setting , -. Recent US data suggest that C. albicans is responsible for 6268% of oropharyngeal Candida spp. infections and 73% of vulvovaginal Candida spp. infections , . C. glabrata and C. dublinensis are leading causes of non-albicans Candida infections in US and South African populations -.
Herpes Simplex Virus Disease
Because acute episodes of herpes simplex virus infection can be treated successfully, chronic therapy with acyclovir is not required after lesions resolve. However, persons who have frequent or severe recurrences can be administered daily suppressive therapy with oral acyclovir or famciclovir .27,28 Valacyclovir is also an option . Intravenous foscarnet or cidofovir can be used to treat infection that is due to acyclovir-resistant isolates of HSV, which are routinely resistant to ganciclovir as well .
Pregnant Women. In patients who have frequent, severe recurrences of genital HSV disease, acyclovir prophylaxis might be indicated . No pattern of adverse pregnancy outcomes has been reported after acyclovir exposure.29
Don’t Miss: Augmentin 875 Dosage For Tooth Infection
Antiretroviral Therapy And Oi Treatment
The indication for antiretroviral therapy in Germany is based on the guidelines by the German and Austrian AIDS Societies . However, general recommendations regarding when to start ART with mostly ART-naïve patients in the setting of an OI cannot be given.
In the case of candidiasis, herpes virus infections or, for example, cryptosporidiosis, the immediate start of ART is uncomplicated in the case of progressive multifocal leukoencephalopathy it is even necessary and recommended. The situation is more difficult in cases of Pneumocystis jiroveci pneumonia , cerebral toxoplasmosis, cytomegalovirus -retinitis, tuberculosis , atypical mycobacteriosis, and cryptococcosis. We refer to the corresponding sections of these guidelines.
The recommendations given here represent the consensus of the guideline consensus group. The recommendations referring to medical therapies might involve off-label therapies that have not been officially approved. This is due to the lack of data from RCTs on HIV-infected patients with OI. In such cases, the recommendation often refers to data on HIV-negative persons or personal experience . It should also be noted that drugdrug interactions or toxicities need to be excluded in each single case.