Who Should Be Vaccinated
Use of the serogroup B meningococcal vaccine falls into two categories. The first is the group of persons identified to be at increased risk because of a serogroup B meningococcal disease outbreak. Based on discussions with the New York City Department of Health and Mental Hygiene and the Centers for Disease Control and Prevention, Columbia Health recommends meningococcal serogroup B vaccination for students enrolled in the School of International and Public Affairs .
The second group is adolescents and young adults who may elect to be vaccinated with MenB vaccines to provide maximum protection against most strains of serogroup B meningococcal disease. These individuals should have an individual appointment with their clinician to determine if vaccination is appropriate.
Vaccination for faculty and staff at Columbia University is also not recommended at this time. Reach out to your healthcare provider if you would like to discuss vaccination further.
Who Should Not Be Immunised
- There are very few people who cannot be given meningococcal vaccines.
- Immunisation should be postponed if a child has a high temperature or serious infection. Minor infections such as coughs, colds and snuffles are no reason to postpone immunisation.
- The vaccine should not be given if there has been a severe reaction to a previous dose of vaccine . Also, it should not be given if a person is known to have a severe allergy to any of the ingredients in the vaccine.
- The vaccines are safe if you are breastfeeding.
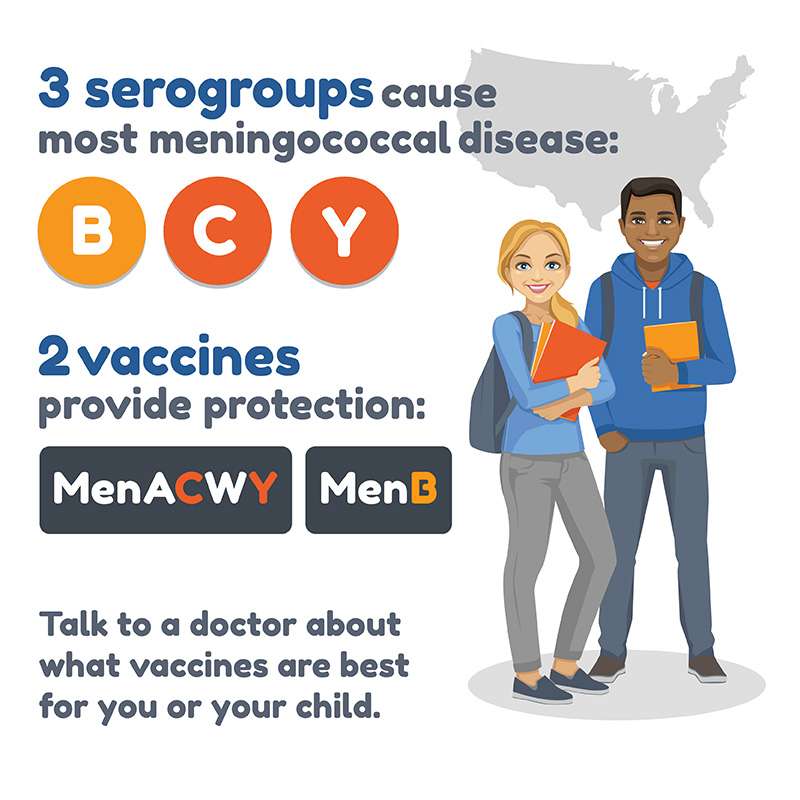
Is There A Vaccine That Will Protect Me From Meningococcal Disease
Yes. There are several vaccines available in the United States. Some vaccines provide protection for four types of meningococcal disease while others provide protection for only one type . All are very safe and effective. Talk to your doctor to find out if you or your family needs the vaccine, and which vaccine is best for you.
Also Check: Can Ear Infection Cause Runny Nose
Are There Any Side
Most people have no side-effects. A mild high temperature may develop for a short time after baby injections. Some babies cry more and become irritable for a short time after the injection. Occasionally they may be sick or have diarrhoea. Slight swelling, pain and redness at the injection site may occur. Headache and muscle aches for a short time can occur in some older children.
None of the above side-effects is serious, and they soon settle. It is a good idea to give your baby a single dose of liquid infant paracetamol at the time of their MenB vaccine or soon after, as a high temperature is a little more common after this vaccine. If necessary, you can give paracetamol or ibuprofen to children to ease pain as well as fever following immunisation. Serious reactions are rare.
Uncommon side-effects, described in up to 1 in 100 people, are high fever, seizures , vomiting dry skin, itchy rash, skin rash, and paleness .
Rare side-effects include Kawasaki syndrome .
What Is The Meningococcus
The meningococcus is a germ that can cause meningitis and blood infection . It can also cause other infections – for example, pneumonia, eye infection , joint infection and inflammation of the heart . It most commonly causes infections in babies under the age of 1 year. It can also cause infections in those aged 1-5 years and those aged 15-19 years.
Some of these infections are very serious and can be fatal if not treated quickly. There are different groups of meningococcal bacteria:
- Groups B, C and, more recently, W are the common strains in the UK. Most cases of bacterial meningitis in the UK are caused by group B. Most of the rest are caused by group C . Infection caused by group W has increased in the UK in recent years.
- Group A is rare in the UK but more common in certain parts of the world – in particular, sub-Saharan Africa and parts of Saudi Arabia.
- Groups Y, 29E and Z are rare in the UK but group W has been the cause of several recent outbreaks in different parts of the world, including the UK.
Infection with the meningococcus can affect anyone but those most at risk are children aged under 5 years , teenagers and young adults under the age of 25.
Don’t Miss: Natural Cure For Yeast Infection On Skin
Two Types Of Meningitis Vaccine:
Two categories of meningitis vaccine are available at UHS, quadrivalent vaccine and meningitis B vaccine.
Quadrivalent vaccine is routinely recommended for our incoming first-year students, especially for those living in residence halls:
- Protects against four strains , which cause 2/3 of meningitis cases
- Brand names are Menactra, Menomune and Menveo
- Recommended for adolescents 11-18 years old and certain others first-year college students living in residence halls are at increased risk of disease
- For more information including side effects and contraindications, see CDC Vaccine Information Statement
Meningitis B vaccine expands protection against this serious but rare infection.
-
People ages 16 -23 years old are eligible to receive this vaccine, and ages 16 -18 years are the preferred ages for vaccination.
-
People 10 years or older who are at increased risk are recommended to receive the vaccine, including:
- People at risk because of a serogroup B meningococcal disease outbreak
- Anyone whose spleen is damaged or has been removed
- Anyone with a rare immune system condition called persistent complement component deficiency
- Anyone taking a drug called eculizumab
- Microbiologists who routinely work with isolates of N. meningitidis
The vaccine:
- Protects against strain B, which causes 1/3 of meningitis cases
- Brand names are Bexsero and Trumenba, which are both offered at UHS.
- Is relatively expensive, so be sure to check whether it is covered by your health insurance.
What Are The Symptoms Of Meningococcal Disease
Although most people exposed to the meningococcus bacteria do not become seriously ill, some may develop fever, headache, vomiting, and a stiff neck. Other symptoms may include nausea, confusion and sensitivity to light. Later in the illness, a rash that looks like purple blotches or spots on the arms, legs and torso may appear.
Read Also: Can Hiv Cause Ear Infection
What Are The Risks From Meningococcal Vaccine
Most people have mild side effects from the vaccine, such as redness or pain where the shot was given. A vaccine, like any medicine, may cause serious problems, such as severe allergic reactions. This risk is extremely small. Getting the meningococcal vaccine is much safer than getting the disease.
You can learn more on the Vaccine Information Statements for meningococcal ACWY and meningococcal B.
Who Should Get The Meningococcal Vaccines
All children ages 11 through 12 years should receive meningococcal vaccine followed by a booster dose at age 16 years. Vaccination is also recommended for all adolescents ages 13 through 18 years who did not receive a dose at age 11-12 years.
Individuals ages 2 months and older who have certain conditions that weaken their immune system should receive meningococcal vaccine, including teens who are HIV positive. These persons should also receive booster shots every three to five years depending on their age. Talk to your health care provider if your preteen or teen has a condition that makes it harder for their body to fight off infection.
The MenB vaccine may also be given at age 16 years along with the MenACWY booster dose. MenB vaccine is also recommended for children age 10 years and older with certain high-risk conditions. The number of doses needed depends on the product used and if your child has a high-risk condition. Talk to your health care provider about this additional vaccine.
Recommended Reading: Boric Acid For Urinary Tract Infection
Why Are Meningococcal Vaccines Recommended
Meningococcal disease is caused by a type of bacteria. It can lead to an infection of the bloodstream or meningitis, or both, and can be life-threatening if not quickly treated. The MenACWY vaccine is very effective at protecting against four strains of the bacteria, while the MenB vaccine protects against a fifth strain.
Global Public Health Response Elimination Of Meningococcal A Meningitis Epidemics In The African Meningitis Belt
In the African meningitis belt, meningococcus serogroup A accounted for 8085% of meningitis epidemics before the introduction of a meningococcal A conjugate vaccine through mass preventive campaigns and into routine immunization programmes . As of April 2021, 24 of the 26 countries in the meningitis belt have conducted mass preventive campaigns targeting 1-29 year olds , and half of them have introduced this vaccine into their national routine immunization schedules. Among vaccinated populations, incidence of serogroup A meningitis has declined by more than 99% – no serogroup A case has been confirmed since 2017. Continuing introduction into routine immunization programmes and maintaining high coverage is critical to avoid the resurgence of epidemics.
Cases of meningitis and outbreaks due to other meningococcal serogroups, apart from serogroup B, continue to strike. The roll out of multivalent meningococcal conjugate vaccines is a public health priority to eliminate bacterial meningitis epidemics in the African Meningitis Belt.
Pneumococcus
The pneumococcus has over 97 serotypes, 23 causing most disease.
Haemophilus influenzae
Haemophilus influenzae has 6 serotypes, serotype b causing most meningitis.
- Conjugate vaccines protect specifically against Haemophilus influenzae serotype b . They are highly effective in preventing Hib disease and are recommended for routine use in infant vaccine schedules.
Group B streptococcus
Don’t Miss: Best Antibiotic For Foot Infection
Is The Meningitis B Vaccine Safe
In the same 2021 study mentioned above, researchers found the vaccine demonstrated an acceptable level of safety. No safety concerns have been raised based on current data, which includes more than 3 million doses administered in the United Kingdom.
Data from Quebec revealed four cases of a kidney disorder called nephrotic syndrome in children age 2 to 5 within 13 months of receiving their vaccine. Researchers are still trying to understand if theres a link, but a lack of similar findings from other countries suggests these cases may have occurred by chance.
Side effects of meningitis B are usually mild and last for
Meningococcal Disease: What It Is And How To Prevent It
What is meningococcal disease?
Meningococcal disease is any infection caused by the bacterium Neisseria meningitidis. It can cause bloodstream infections or meningitisan inflammation in the lining that covers the brain and spinal cord. The type of meningitis that is caused by meningococcal disease is referred to as meningococcal meningitis. It will strike otherwise healthy individuals and can cause devastating illnesseven death.
Death can occur in as little as a few hours. In non-fatal cases, permanent disabilities can include hearing loss, brain damage, and loss of fingers or toes. The Centers for Disease Control and Prevention recommends that all preteens and teens get the meningococcal vaccine.
How does meningococcal disease spread?
Meningococcal disease is spread from person to person. The bacteria are spread by exchanging saliva with someone who has meningococcal disease or who is a carrier. Its possible to get it by kissing, sharing drinking glasses or toothbrushes, or being in very close contact while coughing. It is not spread by casual contact or by simply breathing the air where a person with meningococcal disease has been.
What are symptoms of meningococcal meningitis?
What are symptoms of a bloodstream infection?
Who is at risk for meningococcal disease?
The following people are at high-risk for meningococcal disease and should get vaccinated:
How can you prevent meningococcal disease?
Additional resources
Read Also: Metronidazole For Tooth Infection Dosage
Muslims Undergoing The Hajj Or Umrah Pilgrimage
Pilgrims to Saudi Arabia are especially at risk of contracting meningococcal infection. There have been outbreaks in recent years. A proof of immunisation is needed to obtain a visa to go to Saudi Arabia for this purpose.
Note: some pilgrims may have been immunised in the past with an older vaccine which only protected against groups A and C. If you travel to Saudi Arabia again you should have an injection of the newer MenACWY vaccine. Proof of immunisation with MenACWY vaccine given within the preceding three years is now needed to get a new visa to visit Saudi Arabia.
How Does The Vaccine Work
The vaccine is made from parts of dead meningococcal bacteria. The vaccine helps your body build its defense against future infections. Your defense system includes antibodies. Your body makes these to fight specific infections. This shot helps your body make the right antibodies that fight off meningococcal disease. The vaccine prevents many types of meningococcal infections. It doesnt protect against all of them. You can’t become infected with the disease by getting the shot.
You May Like: Can I Get Rid Of A Sinus Infection Without Antibiotics
When Are Meningococcal Vaccines Given
Vaccination with MenACWY is recommended:
- when kids are 11 or 12 years old, with a booster given at age 16
- for teens 1318 years old who haven’t been vaccinated yet
Those who have their first dose between the ages of 1315 should get a booster dose between the ages of 1618. Teens who get their first dose after age 16 won’t need a booster dose.
Kids and teens who are at higher risk for meningococcal disease need the full series of MenACWY vaccines, even if they’re younger than 11 years old. This includes kids who:
- live in or travel to countries where the disease is common
- are present during an outbreak of the disease
- have some kinds of immune disorders. If the immune disorders are chronic, these kids also need a booster dose a few years later, depending on their age at the first dose.
The sequence and dosage depends on the child’s age, medical condition, and vaccine brand. Some types of meningococcal vaccines can be given as early as 8 weeks of age.
Kids 10 years and older with these risk factors also should get the MenB vaccine. They’ll need 2 or 3 doses depending on the brand. They might need more booster doses as long as the risk factor remains.
For those without risk factors, the decision to receive the MenB vaccine should be made together by teens, their parents, and the doctor. For them, the preferred age range is 1618 years. Usually, they need 2 doses.
Who Should Get The Vaccine
Meningococcal vaccine is recommended for:
- Teens going to certain countries, including parts of Africa
- College students
- Teens living close together, such as in a dorm on a college campus or in military barracks
- Teens with weak immune systems or who take medicines that weaken the immune system
- Teens who don’t have a spleen, or their spleen does not work right
- Students who work with or study meningococcal diseases in the lab
The vaccine is not recommended if you:
- Had a bad reaction before to the meningococcal vaccine
- Are moderately or severely ill
Also Check: How To Get Antibiotics For Sinus Infection
When To Get Vaccinated
The key to the meningitis vaccines is to make sure that your teen gets them at the right time. Your child may get the MCV4 vaccine if they are:
- Between 11 and 15 years old. After the initial MCV4 vaccine, your teen will get a booster shot after five years.
- After the age of 16. In this case, your teen wont need the booster shot. Important to note: Its better to get the vaccines earlier rather than later. This will help prevent meningitis during your teens high school years.
- First-year college students. This applies to those who havent received a diagnosis or missed their booster shots.
- Those deemed by a pediatrician to need extra protection. This is due to underlying illnesses. Examples include immune system disorders or a damaged spleen.
Technically, the MenB vaccine is approved for children over the age of 10. Your doctor might recommend a dose at a younger age if your child has immune system deficiencies. But MenB is usually taken around the age of 16. The American Academy of Pediatrics recommends MenB shots for teens ages 16 to 18. However, it may be given to young adults up to 23 years old.
Vaccines Reduce Number Of Meningitis Infections But For How Long
Jan. 9, 2001 — Bacterial meningitis, an often devastating infection resulting in inflammation of the spinal cord and the fluid surrounding the cord and the brain, can cause death, brain damage, hearing loss, severe learning disabilities, and many other potentially devastating conditions. Infants, adolescents, and young adults are most susceptible to infection.
But parents and others who care for children and teens will be relieved to hear that two recent studies have given a big shot in the arm to meningitis prevention efforts. Last week, the British government announced that an aggressive immunization program using a new vaccine against a particularly virulent form of bacterial meningitis, meningitis C, reduced the number of new meningitis cases in the U.K. by up to 90%. And now Canadian researchers report similar success with a mass immunization campaign in the province of Quebec in 1992-1993.
Unlike the new vaccine used in the U.K., however, the vaccine type still in use in both Canada and in the U.S. appears to protect children and teens for only a few years, and infants under 2 get almost no protection, say Phillipe De Wals, PhD, and colleagues in the Jan. 10 issue of the Journal of the American Medical Association.
Show Sources
Read Also: Betadine Soak For Infected Finger
How Does Meningococcal Disease Spread
Meningococcal disease is spread by contact with spit, phlegm, or other fluids from the nose or mouth of someone who has the disease. Someone who has had close contact with an infected person can become infected, but taking the correct antibiotic right away can prevent illness.
Close contact includes:
- Sneezing, or coughing on someone
- Living in a crowded space, such as in dormitories
- Sharing eating or drinking utensils or other items placed in the mouth or nose
A person with meningococcal disease can spread infection to others 7 days before they feel sick, and while they are sick until 24 hours after the start of appropriate antibiotics.