General Guidelines For Prophylaxis
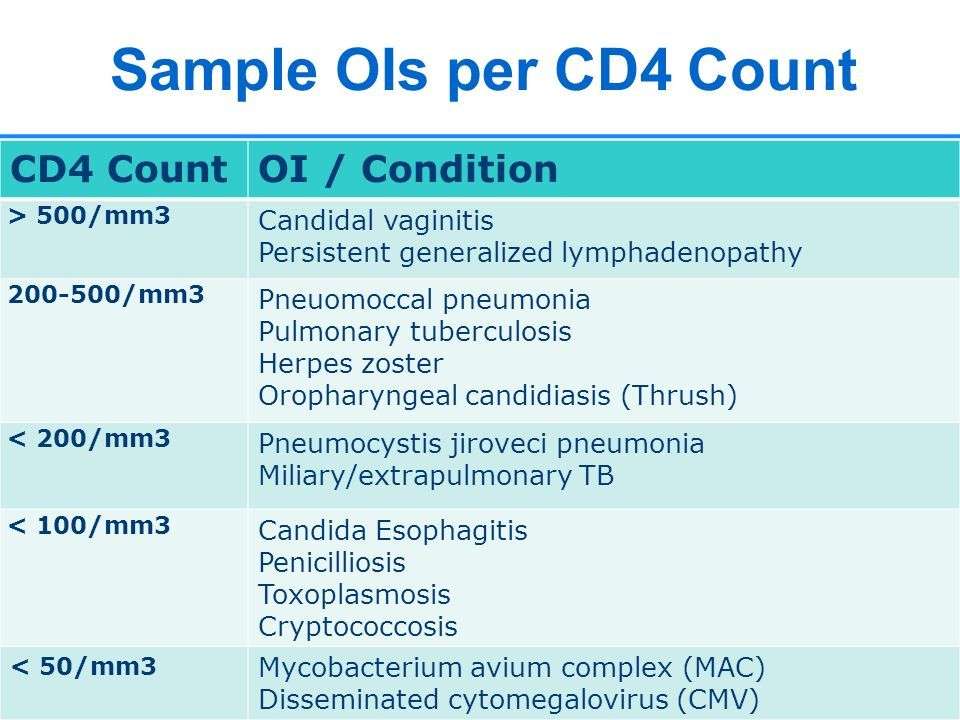
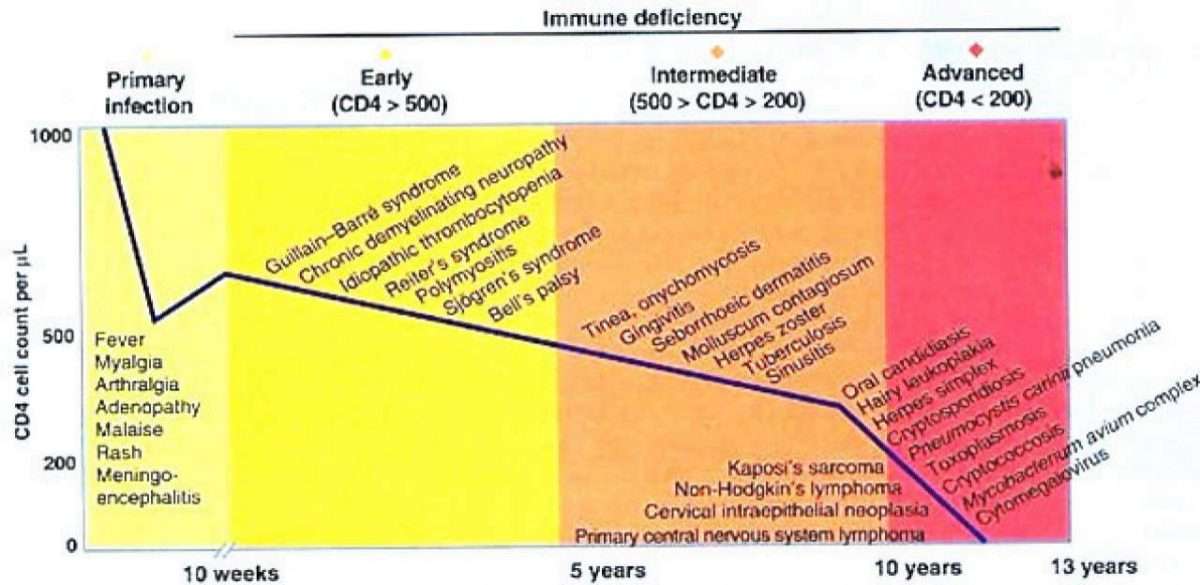
Immunosuppression resulting from HIV places a patient at risk for infection from organisms that are otherwise relatively mildly hazardous and that would normally be cleared by a competent immune system. For many years before the development of effective antiretroviral therapy , these infections inflicted significant morbidity and mortality on patients living with AIDS. They generally include Pneumocystis jiroveci pneumonia , toxoplasma encephalitis, cryptococcal meningitis, cytomegalovirus retinitis, tuberculosis , disseminated Mycobacterium avium complex , or pneumococcal respiratory disease.
Prevention of opportunistic infections in patients with HIV has since significantly reduced morbidity and mortality in these patients. HIV-related infections and malignancies escalate in frequency and severity as the absolute CD4 T cell count falls toward 200 cells/L and below. This risk is more prominent in patients with lower CD4 counts as well as in patients with a longer time spent with more severe immunosuppression however, it is also seen more severely in patients not on ART. Patients should be aware of their CD4 count and their risk for specific infections and should begin ART.
The recommendations below use evidence-based criteria as published by the joint CDC/NIH/IDSA that summarize the strength of the recommendation and quality of the evidence :
Strength of recommendation is as follows:
A: Strong recommendation for the statement
B: Moderate recommendation for the statement
Having A Diagnosis Of Aids
Acquired immune deficiency syndrome is the name used to describe a range of illnesses which can develop when someones immune system has been significantly weakened by HIV.
Depending on where you live, the way an AIDS diagnosis is given will vary. In some countries, someone will be given an AIDS diagnosis if they develop an AIDS-related illness. In others you will be given an AIDS diagnosis if your CD4 count is below 200.
Being diagnosed with AIDS does not mean that your health will continue to deteriorate. Many people diagnosed with AIDS have become healthy again, with good treatment and care.
Adult/adolescent Spectrum Of Hiv Disease Project
The Adult and Adolescent Spectrum of HIV Disease Investigators are Melanie Thompson, M.D., Julia Gable, M.S., and William McCarthy, Ph.D., AIDS Research Consortium of Atlanta, Atlanta, GA Sylvia Odem, M.P.H., and Sharon Melville, M.D., Texas Department of Health, Austin Arthur J. Davidson, M.D., David L. Cohn, M.D., and Cornelius A. M. Rietmeijer, M.D., Denver Department of Health and Hospitals, Denver, CO Linda L. Wotring, Ph.D., M.P.H., and Eve D. Mokotoff, M.P.H., Michigan Department of Community Health, Detroit Wes McNeely, M.S., and Kaye Reynolds, Houston Department of Health and Human Services, Houston, TX Frank Sorvillo, Ph.D., and Dorothy Masters, Los Angeles County Department of Health Services, Los Angeles, CA Anne Morse and Stephanie Broyles, M.P.H., Louisiana Office of Public Health, New Orleans Judy Sackoff, Ph.D., and Jeffrey McFarland, M.D., The City of New York Department of Health, New York, NY Jose Otero, M.P.H., Robert Hunter, M.D., and Maria de los Angeles Gomez, Ph.D., University Central del Caribe, Bayamon, and Sandra Miranda, M.P.H., Puerto Rico Department of Health, San Juan Susan Buskin, Ph.D., Sharon G Hopkins, D.V.M., and Beth Sohlberg, M.S., Seattle King County Department of Public Health, Seattle, WA.
Don’t Miss: Sexually Transmitted Infections And Hiv
Cd4 Count Vs Viral Load
Theres no direct relationship between CD4 count and viral load.
In the past, doctors used the CD4 count as an indicator of when to start therapy, but advances in HIV medication have changed this. Now it serves as an indicator of immune system stability.
However, in general, a high CD4 count and a low or undetectable viral load are desirable. The higher the CD4 count, the healthier the immune system. The lower the viral load, the likelier it is that HIV therapy is working.
When HIV invades healthy CD4 cells, the virus uses them to make new copies of HIV before destroying them. When HIV remains untreated, the CD4 count decreases, and the viral load increases.
The following chart gives a general idea of what the levels of CD4 and viral load mean for a person with HIV, based on guidelines from the U.S. Department of Health and Human Services.
| How serious is this? |
| After levels remain stable for 2 years. | Up to 6 months interval |
Association Between Nadir Cd4 T
A ROC analysis was used to study the association between nadir CD4 T-cell count within the first three months post-transplantation and the frequency of infectious episodes within the successive six month period. Although no significant differences in the number of infectious episodes were observed between LTR with a nadir CD4 T-cell count < 200 cells/l and those with a nadir CD4 T-cell count > 200 cells/l , the number of infectious episodes in LTR with a nadir CD4 T-cell count < 200 cells/l was significantly higher than in LTR with a nadir CD4 T-cell count > 200 cells/l .
Association between nadir CD4 T-cell count and subsequent infectious episodes. Relationship between lung transplant recipients with a nadir CD4 T-cell count < 200 cells/l or > 200 cells/l within the first three months post-transplantation and the number of infectious episodes detected in blood or BAL samples within the successive six month period. P values are depicted for each graph p < 0.05 was considered statistically significant.
Read Also: Should You Go To The Doctor For An Ear Infection
What Is A Viral Load
An HIV viral load test measures the number of HIV particles in a milliliter of blood. These particles are also known as copies. The test assesses the progression of HIV in the body. Its also useful in seeing how well a persons HIV therapy is managing the virus in their body.
A person may have a high viral load soon after contracting HIV or if treatment is not proving effective. When a person first contracts the virus, levels will rise significantly, but in the next 3 to 8 weeks, the body starts to produce antibodies. This can reduce the virus levels. A viral load can include copies per mL of blood, especially after recent exposure, according to an observational study of data published in 2018.
Effective treatment will result in viral suppression. This is when there are fewer than 200 copies/mL. At this stage, the risk of HIV progressing is low, but the virus is still present A person can still pass on the virus.
As treatment progresses, the viral load can become so low that it is undetectable in a test. An undetectable viral load will be under 40 to 75 copies in a blood sample. This means there are relatively few copies of HIV in the blood.
When this happens, it is no longer possible to pass the virus on to another person during sex, according to the . An undetectable amount of HIV is untransmittable.
However, continued treatment is necessary to ensure the viral load remains undetectable.
Distribution Of Bacterial Growth And Fungal Growth In Hiv
Among bacterial growth, 91.6% were mono-microbial and 8.4% were poly-microbial, among which, Klebsiella pneumoniae was predominant, followed by Pseudomonas aeruginosa . Among 42 fungal growths, yeast was isolated from 29 samples , only molds were isolated from 12 samples and both yeast and mold were isolated from one sample . One patient was found to be co-infected with more than one fungus.
|
Table 1 Culture Results of Sputum Samples of HIV Patients |
Out of a total of 30 isolates of yeast, six different species of yeast were identified. Candida albicans, 20 , was the most predominant organism followed by Candida parapsilosis,4 . Out of a total of 13 mold isolates, four different types of molds: Aspergillus flavas, Aspergillus fumigatus,Penicillium spp. and Mucorspp. were identified. Aspergillus spp., 6 , were the most predominant organism followed by Penicillium spp., 5 and Mucor spp., 2 .
Read Also: Baby Ear Infection Vs Teething
Opportunistic Infections In Hiv Infected Children And Its Correlation With Cd4 Count
Ravichandra K. R., Bikash Ranjan Praharaj, Sunil Agarwalla
Abstract
Background: HIV infected children usually have higher viral load, weaker immune system, variable latency period, fewer opportunistic infections and fewer medicines approved for management. Knowledge of the clinical profile in HIV infected children will help in better understanding of the disease and management. The present study was aimed to study the clinical presentation, opportunistic infections, WHO clinical stage, nutritional status and its correlation with CD4 count.
Methods: 50 children below 14 years of age and seropositive for HIV were included in this study and were categorized into WHO clinical stages. They were further classified based on CD4 count values in accordance with WHO classification of immunodeficiency.
Results: In the study 30% of children were in the age group of 4 to 7 years. The mean age of presentation was 7.12 years. 56% of children presented with WHO clinical stage III and 30% with stage IV at first visit. Vertical transmission was the predominant mode of transmission. Anaemia , fever and cough were common symptoms. Pulmonary tuberculosis was the most common opportunistic infection seen at mean CD4 count of 267±5.37.
Keywords
Diminished Generation Of T
Investigations of the bone marrow of five ICL patients revealed that the percentage of phenotypically primitive CD34+CD38DR+ cells was decreased, suggesting an involvement of the more primitive bone marrow compartment in de novo T-cell generation. This raises the possibility that the diminished availability of stem cell precursors might contribute to the development of CD4+ T-cell depletion in ICL patients .
Recommended Reading: Over The Counter Antibiotics For Bladder Infection
Enhancing Healthcare Team Outcomes
HIV patients who are untreated are prone to multiple opportunistic infections due to the progressive lowering of their CD4 + T cells. Because of the high morbidity and mortality of these infections, every attempt should be made that these patients have enough resources for early diagnosis of HIV, timely initiation of ART, regular follow up to ensure medication adherence.
These patients should be managed by an interprofessional team that includes an infectious disease specialist, internist, specialist nurse, pharmacists, and social workers. They also need close monitoring with regular lab work to evaluate for improvement of CD4+ cell count, assessment of medication-related side effects, and the emergence of opportunistic infections. Patients with HIV often face social stigma due to their infections. The team must additionally ensure adequate social and financial support, rehabilitation for intravenous drug abusers along with patient education regarding safe sex practices, and avoidance of high-risk behaviors.
Prophylaxis And Treatment Of Opportunistic Infections
When CD4 counts fall below 200 cells µL1, patients with HIV are at risk for opportunistic infections . Guidelines for patients with ICL are not available, and thus the current recommendations are based mainly on experience with HIV-infected patients. Prophylaxis against pneumocystis is recommended when CD4 T-cell counts fall below 200 cells µL1. Cryptococcus as well as relapsing multisegmental herpes infection may require lifelong secondary prophylaxis. Antimycobacterial medication has been reported to produce improvement of CD4 T-cell counts in CD4 lymphocytopenia with mycobacterial infections .
Also Check: Best Treatment For Male Urinary Tract Infection
Management Of Opportunistic Infections
Identification of opportunistic infections: Tuberculosis Except as specifically described below for people with HIV infection with low CD4 counts or who are seriously ill, urine lateral flow -LAM should not be used for the diagnosis of TB.12
LF-LAM may be used to assist in the diagnosis of active TB in adult inpatients living with HIV, with signs and symptoms of TB , who have a CD4 count less than or equal to 100 cells/µl, or people living with HIV who are seriously ill, regardless of CD4 cell count or with unknown CD4 cell count.12 LF-LAM should not be used as a screening test for active TB.12
Identification of opportunistic infections: Cryptococcus spec.The use of routine serum or plasma Cryptococcus antigen screening in ART-naive adults, followed by pre-emptive antifungal therapy if CrAg positive to reduce the development of cryptococcal disease, may be considered prior to ART initiation in:13
a. patients with a CD4 count less than 100 cells/µl and
b. where this population also has a high prevalence of cryptococcal antigenaemia.
Identification of opportunistic infections: Skin and oral conditionsHIV infection increases the prevalence and severity of skin and oral diseases, especially when the persons CD4 count declines below 200 cells/µl. As a result, skin and oral conditions affect up to 90 percent of adults and children with HIV in resource-limited settings.14
Identification Of Fungal Isolates
For isolation of fungal pathogens, sputum samples were inoculated in duplicate Sabouraud`s Dextrose Agar tubes and incubated at room temperatures: 25ºC and 37ºC. The cultures were examined on alternate days for growth and were kept for 21 days before discarding them as negative.25 Fungal isolates were identified macroscopically and microscopically based on the colonial morphology of the isolates on the laboratory media. Mucoid yeast-like growth was processed by carrying out Grams staining and capsular staining, germ tube test and urease test. Grams staining was done to all the isolates with mucoid- and yeast-like growth and observed for Gram-positive budding yeast cells.5,15
Don’t Miss: Can You Use Keflex For Tooth Infection
You Are Reading A Preview
Activate your 30 day free trial to continue reading.
Cumulative Incidence Of Viral Infections Stratified By Nadir Cd4 T
In LTR with a nadir CD4 T-cell count < 200 cells/l, the cumulative incidence of infections in blood was 61%, while in LTR with a nadir CD4 T-cell count > 200 cells/l it was 29% . The cumulative incidence of infections in BAL was significantly higher in LTR with a nadir CD4 T-cell count < 200 cells/l than in LTR with a nadir CD4 T-cell count > 200 cells/l .
Cumulative incidence of viral infections in 83 lung transplant recipients in the first 1213 months post-transplant stratified by nadir CD4 T-cell count . Viral infections detected in peripheral blood samples . Viral infections detected in BAL samples . P values are depicted for each graph p < 0.05 was considered statistically significant.
Read Also: Best Over The Counter Yeast Infection Pill
What Causes A Cd4 Count To Drop
CD4 cells are part of the immune system. They are present in blood cells and help protect the body from disease. When HIV enters body cells, it reproduces or makes copies of itself. As it does so, it causes CD4 cells to die, leaving the body more prone to infection and disease.
Typically, the more virus thats in the body, the lower the levels of CD4 will be, the more the immune system will be compromised, and the higher the persons risk of infection.
Antiretroviral treatment suppresses the virus and gives CD4 cells a chance to recover. As a person receives treatment, they can expect CD4 levels to rise. In the first year of antiretroviral treatment, you can expect typically to see a persons CD4 count rise by 50150 cells/mm3. After that, there will be slower yearly increases.
Opportunistic Infections And Cd4 Levels
The prevalence of OIs was found to be highest among HIV-infected patients with CD4 count less than 200/mm3 followed by CD4 count 200-350/mm3 and count above 350/mm3 with prevalence of and respectively. CD4 count less than 200/mm3 is found to have strong association with acquisition of OIs . Higher prevalence of tuberculosis , diarrhea , oral candidiasis , skin fungal infections , pneumonia and others were found in patients with CD4 count less than 200/mm3. Each OI diagnosed showed strong association with CD4 count less than 200/mm3 oral candidiasis , tuberculosis , skin fungal infections and pneumonia .
Recommended Reading: Frequent Uti And Kidney Infections
What Does Hiv Do To Cd4 Cells
HIV damages your immune system because it targets CD4 cells. The virus grabs on to the surface of a cell, gets inside, and becomes a part of it. When the infected CD4 cell dies, it releases more copies of HIV into the bloomstream.
Those new bits of virus find and take over more CD4 cells, and the cycle continues. This leads to fewer and fewer HIV-free, working CD4 cells.
HIV can destroy entire “families” of CD4 cells, and then the germs these cells fight have easy access to your body. The resulting illnesses are called opportunistic infections because they take advantage of your body’s lack of defense.
Inclusion And Exclusion Criteria
A patient was enrolled in this study if he/she was HIV positive and attended STIDH was clinically diagnosed to have lower respiratory tract infections based on the national treatment guidelines and provided written informed consent regardless of their ART status. People living with HIV/AIDS who were below 15 years of age were excluded from the study.
Read Also: Will Amoxicillin Cure A Sinus Infection
What Else Can Affect Your Cd4 Count
Things other than the HIV virus can influence how high or low your CD4 count is, too.
An infection like the flu, pneumonia, or a herpes simplex virus can make your CD4 count go down for a while.
Your CD4 count will go way down when you’re having chemotherapy for cancer.
To get the most accurate and helpful results for your CD4 count, try to:
- Use the same lab each time.
- Wait for at least a couple of weeks after you’ve been sick or gotten a shot before you get a test.